Discover Ground Truths
Ground Truths

29 Episodes
Reverse
“Where do I think the next amazing revolution is going to come? … There’s no question that digital biology is going to be it. For the very first time in our history, in human history, biology has the opportunity to be engineering, not science.” —Jensen Huang, NVIDIA CEOAviv Regev is one of the leading life scientists of our time. In this conversation, we cover the ongoing revolution in digital biology that has been enabled by new deep knowledge on cells, proteins and genes, and the use of generative A.I .Transcript with audio and external linksEric Topol (00:05):Hello, it's Eric Topol with Ground Truths and with me today I've really got the pleasure of welcoming Aviv Regev, who is the Executive Vice President of Research and Early Development at Genentech, having been 14 years a leader at the Broad Institute and who I view as one of the leading life scientists in the world. So Aviv, thanks so much for joining.Aviv Regev (00:33):Thank you for having me and for the very kind introduction.The Human Cell AtlasEric Topol (00:36):Well, it is no question in my view that is the truth and I wanted to have a chance to visit a few of the principal areas that you have been nurturing over many years. First of all, the Human Cell Atlas (HCA), the 37 trillion cells in our body approximately a little affected by size and gender and whatnot, but you founded the human cell atlas and maybe you can give us a little background on what you were thinking forward thinking of course when you and your colleagues initiated that big, big project.Aviv Regev (01:18):Thanks. Co-founded together with my very good friend and colleague, Sarah Teichmann, who was at the Sanger and just moved to Cambridge. I think our community at the time, which was still small at the time, really had the vision that has been playing out in the last several years, which is a huge gratification that if we had a systematic map of the cells of the body, we would be able both to understand biology better as well as to provide insight that would be meaningful in trying to diagnose and to treat disease. The basic idea behind that was that cells are the basic unit of life. They're often the first level at which you understand disease as well as in which you understand health and that in the human body, given the very large number of individual cells, 37.2 trillion give or take, and there are many different characteristics.(02:16):Even though biologists have been spending decades and centuries trying to characterize cells, they still had a haphazard view of them and that the advancing technology at the time – it was mostly single cell genomics, it was the beginnings also of spatial genomics – suggested that now there would be a systematic way, like a shared way of doing it across all cells in the human body rather than in ways that were niche and bespoke and as a result didn't unify together. I will also say, and if you go back to our old white paper, you will see some of it that we had this feeling because many of us were computational scientists by training, including both myself and Sarah Teichmann, that having a map like this, an atlas as we call it, a data set of this magnitude and scale, would really allow us to build a model to understand cells. Today, we call them foundational models or foundation models. We knew that machine learning is hungry for these kinds of data and that once you give it to machine learning, you get amazing things in return. We didn't know exactly what those things would be, and that has been playing out in front of our eyes as well in the last couple of years.Spatial OmicsEric Topol (03:30):Well, that gets us to the topic you touched on the second area I wanted to get into, which is extraordinary, which is the spatial omics, which is related to the ability to the single cell sequencing of cells and nuclei and not just RNA and DNA and methylation and chromatin. I mean, this is incredible that you can track the evolution of cancer, that the old word that we would say is a tumor is heterogeneous, is obsolete because you can map every cell. I mean, this is just changing insights about so much of disease health mechanisms, so this is one of the hottest areas of all of life science. It's an outgrowth of knowing about cells. How do you summarize this whole era of spatial omics?Aviv Regev (04:26):Yeah, so there's a beautiful sentence in the search for lost time from Marcel Proust that I'm going to mess up in paraphrasing, but it is roughly that going on new journeys is not about actually going somewhere physically but looking with new eyes and I butchered the quote completely.[See below for actual quote.] I think that is actually what single cells and then spatial genomics or spatial omics more broadly has given us. It's the ability to look at the same phenomenon that we looked at all along, be it cancer or animal development or homeostasis in the lung or the way our brain works, but having new eyes in looking and because these new eyes are not just seeing more of something we've seen before, but actually seeing things that we couldn't realize were there before. It starts with finding cells we didn't know existed, but it's also the processes that these cells undergo, the mechanisms that actually control that, the causal mechanisms that control that, and especially in the case of spatial genomics, the ways in which cells come together.(05:43):And so we often like to think about the cell because it's the unit of life, but in a multicellular organism we just as much have to think about tissues and after that organs and systems and so on. In a tissue, you have this amazing orchestration of the interactions between different kinds of cells, and this happens in space and in time and as we're able to look at this in biology often structure is tightly associated to function. So the structure of the protein to the function of the protein in the same way, the way in which things are structured in tissue, which cells are next to each other, what molecules are they expressing, how are they physically interacting, really tells us how they conduct the business of the tissue. When the tissue functions well, it is this multicellular circuit that performs this amazing thing known as homeostasis.(06:36):Everything changes and yet the tissue stays the same and functions, and in disease, of course, when these connections break, they're not done in the right way you end up with pathology, which is of course something that even historically we have always looked at in the level of the tissue. So now we can see it in a much better way, and as we see it in a better way, we resolve better things. Yes, we can understand better the mechanisms that underlie the resistance to therapeutics. We can follow a temporal process like cancer as it unfortunately evolves. We can understand how autoimmune disease plays out with many cells that are actually bent out of shape in their interactions. We can also follow magnificent things like how we start from a single cell, the fertilized egg, and we become 37.2 trillion cell marvel. These are all things that this ability to look in a different way allows us to do.Eric Topol (07:34):It's just extraordinary. I wrote at Ground Truths about this. I gave all the examples at that time, and now there's about 50 more in the cardiovascular arena, knowing with single cell of the pineal gland that the explanation of why people with heart failure have sleep disturbances. I mean that's just one of the things of so many now these new insights it's really just so remarkable. Now we get to the current revolution, and I wanted to read to you a quote that I have.Digital BiologyAviv Regev (08:16):I should have prepared mine. I did it off the top of my head.Eric Topol (08:20):It's actually from Jensen Huang at NVIDIA about the digital biology [at top of the transcript] and how it changes the world and how you're changing the world with AI and lab in the loop and all these things going on in three years that you've been at Genentech. So maybe you can tell us about this revolution of AI and how you're embracing it to have AI get into positive feedbacks as to what experiment to do next from all the data that is generated.Aviv Regev (08:55):Yeah, so Jensen and NVIDIA are actually great partners for us in Genentech, so it's fun to contemplate any quote that comes from there. I'll actually say this has been in the making since the early 2010s. 2012 I like to reflect on because I think it was a remarkable year for what we're seeing right now in biology, specifically in biology and medicine. In 2012, we had the beginnings of really robust protocols for single cell genomics, the first generation of those, we had CRISPR happen as a method to actually edit cells, so we had the ability to manipulate systems at a much better way than we had before, and deep learning happened in the same year as well. Wasn't that a nice year? But sometimes people only realize the magnitude of the year that happened years later. I think the deep learning impact people realized first, then the single cells, and then the CRISPR, then the single cells.(09:49):So in order maybe a little bit, but now we're really living through what that promise can deliver for us. It's still the early days of that, of the delivery, but we are really seeing it. The thing to realize there is that for many, many of the problems that we try to solve in biomedicine, the problem is bigger than we would ever be able to perform experiments or collect data. Even if we had the genomes of all the people in the world, all billions and billions of them, that's just a smidge compared to all of the ways in which their common variants could combine in the next person. Even if we can perturb and perturb and perturb, we cannot do all of the combinations of perturbations even in one cell type, let alone the many different cell types that are out there. So even if we searched for all the small molecules that are out there, the
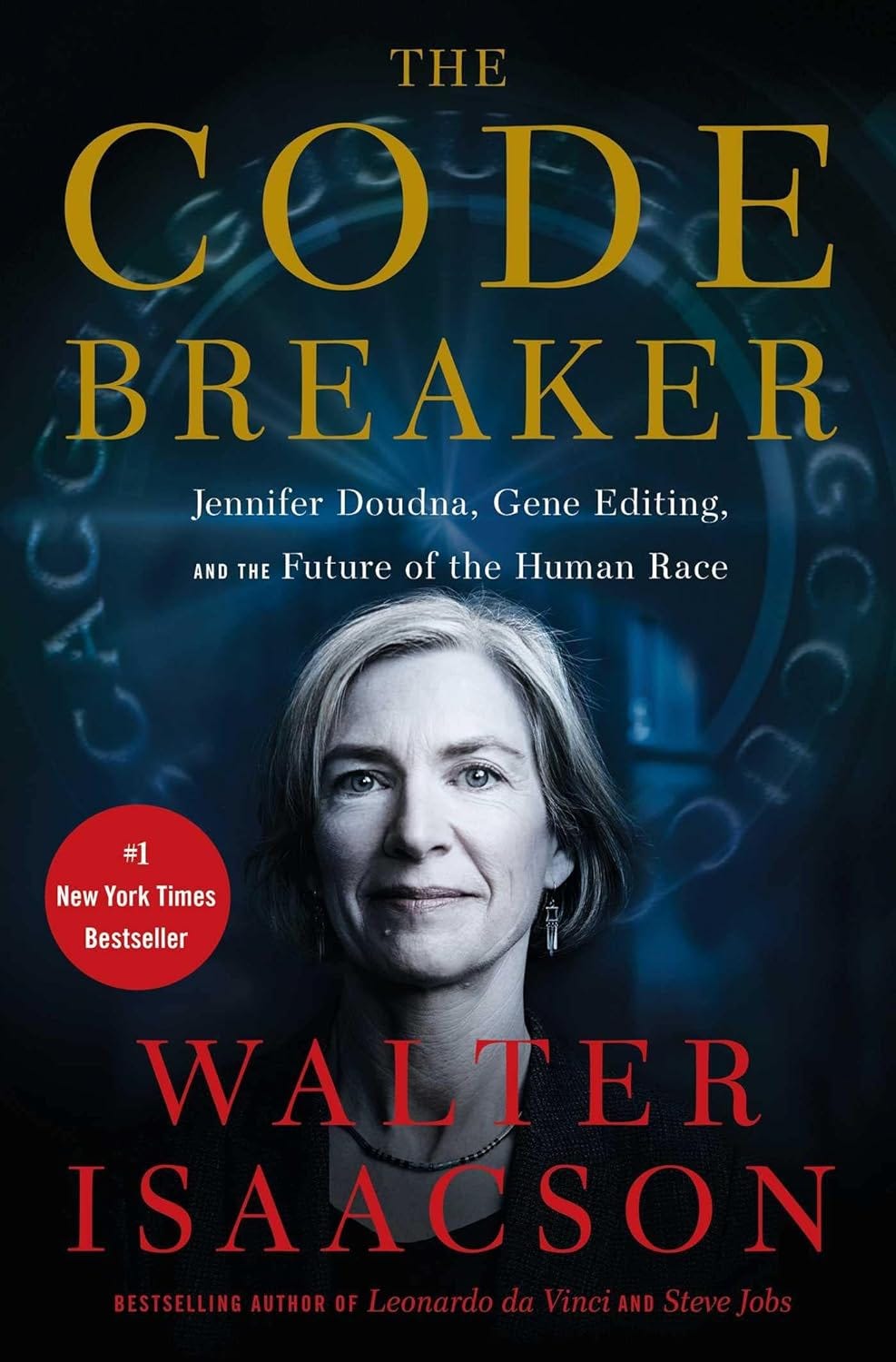
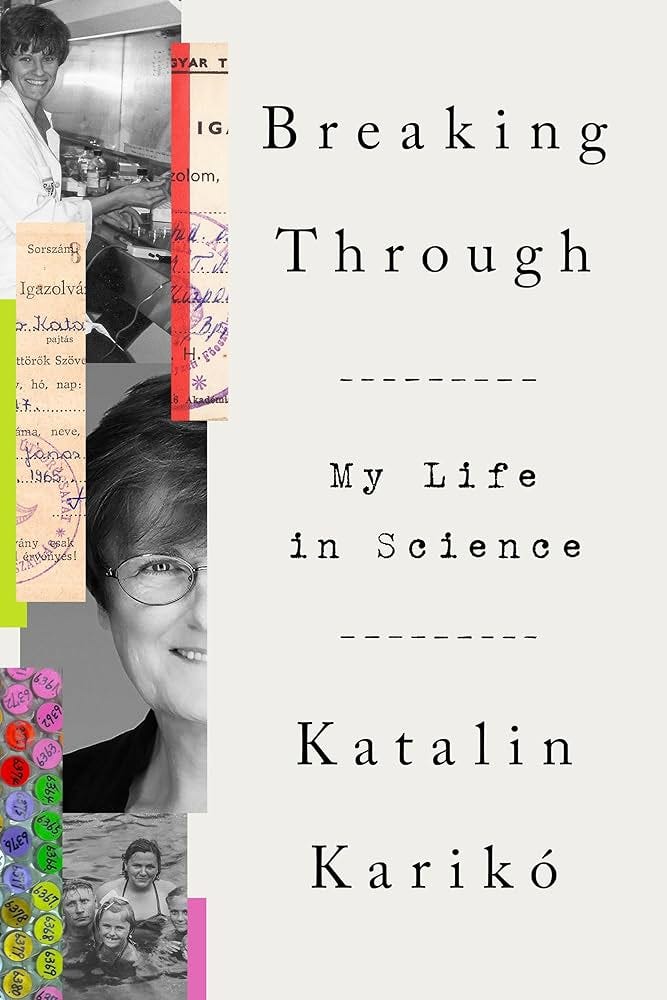
Professor Doudna was awarded the 2020 Nobel Prize in Chemistry with Professor Emmanuelle Charpentier for their pioneering work in CRISPR genome editing. The first genome editing therapy (Casgevy) was just FDA approved, only a decade after the CRISPR-Cas9 editing system discovery. But It’s just the beginning of a much bigger impact story for medicine and life science.Ground Truths podcasts are now on Apple and Spotify. And if you prefer videos, they are posted on YouTubeTranscript with links to audio and relevant external linksEric Topol (00:06):This is Eric Topol with Ground Truths, and I'm really excited today to have with me Professor Jennifer Doudna, who heads up the Innovative Genomics Institute (IGI) at UC Berkeley, along with other academic appointments, and as everybody knows, was the Nobel laureate for her extraordinary discovery efforts with CRISPR genome editing. So welcome, Jennifer.Jennifer Doudna (00:31):Hello, Eric. Great to be here.Eric Topol (00:34):Well, you know we hadn't met before, but I felt like I know you so well because this is one of my favorite books, The Code Breaker. And Walter Isaacson did such a wonderful job to tell your story. What did you think of the book?My interview with Walter Isaacson on The Code Breaker, a book I highly recommendJennifer Doudna (00:48):I thought Walter did a great job. He's a good storyteller, and as you know from probably from reading it or maybe talking to others about it, he wrote a page turner. He actually really dug into the science and all the different aspects of it that I think created a great tale.Eric Topol (01:07):Yeah, I recommended highly. It was my favorite book when it came out a couple years ago, and it is a page turner. In fact, I just want to read one, there's so many quotes out of it, but in the early part of the book, he says, “the invention of CRISPR and the plague of Covid will hasten our transition to the third great revolution of modern times. These revolutions arose from the discovery beginning just over a century ago, of the three fundamental kernels of our existence, the atom, the bit, and the gene.” That kind of tells a big story just in one sentence, but I thought I’d start with the IGI, the institute that you have set up at Berkeley and what its overall goals are.Jennifer Doudna (01:58):Right. Well, let's just go back a few years maybe to the origins of this institute and my thinking around it, because in the early days of CRISPR, it was clear that we were really at a moment that was quite unique in the sense that there was a transformative technology. It was going to intersect with lots of other discoveries and technologies. And I work at a public institution and my question to myself was, how can I make sure that this powerful tool is first of all used responsibly and secondly, that it's used in a way that benefits as many people as possible, and it's a tall order, but clearly we needed to have some kind of a structure that would allow people to work together towards those goals. And that was really the mission behind the IGI, which was started as a partnership between UC Berkeley and UCSF and now actually includes UC Davis as well.The First FDA Approved Genome EditingEric Topol (02:57):I didn't realize that. That's terrific. Well, this is a pretty big time because 10 years or so, I guess starting to be 11 when you got this thing going, now we're starting to see, well, hundreds of patients have been treated and in December the FDA approved the first CRISPR therapy for sickle cell disease, Casgevy. Is that the way you say it?Jennifer Doudna (03:23):Casgevy, yeah.Eric Topol (03:24):That must have felt pretty good to see if you go from the molecules to the bench all the way now to actually treating diseases and getting approval, which is no easy task.Jennifer Doudna (03:39):Well, Eric, for me, I'm a biochemist and somebody who has always worked on the fundamentals of biology, and so it's really been extraordinary to see the pace at which the CRISPR technology has been adopted, and not just for fundamental research, but also for real applications. And Casgevy is sort of the crowning example of that so far, is that it's really a technology that we can already see how it's being used to, I think it's fair to say, effectively cure a genetic disease for the first time. Really amazing.Genome Editing is Not the Same as Gene TherapyEric Topol (04:17):Yeah. Now I want to get back to that. I know there's going to be refinements about that. And of course, there's beta thalassemia, so we've got two already, and our mutual friend Fyodor Urnov would say two down 5,000 to go. But I think before I get to the actual repair of the sickle cell defect molecular defect, I think one of the questions I think that people listeners may not know is the differentiation of genome editing with gene therapy. I mean, as you know, there was recently a gene therapy approval for something like $4.25 million for metachromatic leukodystrophy. So maybe you could give us kind of skinny on how these two fundamental therapies are different.Jennifer Doudna (05:07):Right. Well, it's a great question because the terminology sounds kind of the same, and so it could be confusing. Gene therapy goes back decades, I can remember gene therapy being discussed as an exciting new at the time, direction back when I was a graduate student. That was little while ago. And it refers to the idea that we can use a genetic approach for disease treatment or even for a cure. However, it fundamentally requires some mechanism of integrating new information into a genome. And traditionally that's been done using viruses, which are great at doing that. It's just that they do it wherever they want to do it, not necessarily where we want that information to go. And this is where CRISPR comes in. It's a technology allows precision in that kind of genetic manipulation. So it allows the scientist or the clinician to decide where to make a genetic change. And that gives us tremendous opportunity to do things with a kind of accuracy that hasn't been possible before.Eric Topol (06:12):Yeah, no question. That's just a footnote. My thesis in college at University of Virginia, 1975, I'm an old dog, was prospects for gene therapy in man. So it took a while, didn't it? But it's a lot better now with what you've been working on, you and your colleagues now and for the last decade for sure. Now, what I was really surprised about is it's not just of course, these hemoglobin disorders, but now already in phase two trials, you've got hereditary angioedema, which is a life-threatening condition, amyloidosis, cancer ex vivo, and also chronic urinary tract infections. And of course, there's six more others like autoimmune diseases like lupus and type 1 diabetes. So this is really blossoming. It's really extraordinary.Eric Topol (07:11):I mean, wow. So one of the questions I had about phages, because this is kind of going back to this original work and discovery, antimicrobial resistance is really a big problem and it's a global health crisis, and there's only two routes there coming up with new drugs, which has been slow and not really supported by the life science industry. And the other promising area is with phages. And I wonder, since this is an area you know so well, why haven't we put more, we're starting to see more trials in phages. Why haven't we doubled down or tripled down on this to help the antimicrobial resistance problem?Jennifer Doudna (08:00):Well, it's a really interesting area, and as you said, it's kind of one of those areas of science where I think there was interest a while ago and some effort was made for reasons that are not entirely clear to me, at least it fizzled out as a real focused field for a long time. But then more recently, people have realized that there's an opportunity here to take advantage of some natural biology in which viruses can infect and destroy microbes. Why aren't we taking better advantage of that for our own health purposes? So I personally am very excited about this area. I think there's a lot of fundamental work still to be done, but I think there's a tremendous opportunity there as well.CRISPR 2.0Eric Topol (08:48):Yeah, I sure think we need to invest in that. Now, getting back to this sickle cell story, which is so extraordinary. This is kind of a workaround plan of getting fetal hemoglobin built up, but what about actually repairing, getting to fixing the lesion, if you will?Eric Topol (09:11):Yeah. Is that needed?Jennifer Doudna (09:13):Well, maybe it's worth saying a little bit about how Casgevy works, and you alluded to this. It's not a direct cure. It's a mechanism that allows activation of a second protein called fetal hemoglobin that can suppress the effect of the sickle cell mutation. And it's great, and I think for patients, it offers a really interesting opportunity with their disease that hasn't been available in the past, but at the same time, it's not a true cure. And so the question is could we use a CRISPR type technology to actually make a correction to the genetic defect that directly causes the disease? And I think the answer is yes. The field isn't there quite yet. It's still relatively difficult to control the exact way that DNA editing is occurring, especially if we're doing it in vivo in the body. But boy, many people are working on this, as you probably know. And I really think that's on the horizon.Eric Topol (10:19):Yeah. Well, I think we want to get into the in vivo story as well because that, I think right now it's so complicated for a person to have to go through the procedure to get ultimately this treatment currently for sickle cell, whereas if you could do this in vivo and you could actually get the cure, that would be of the objective. Now, you published just earlier this month in PNAS a wonderful paper about the EDVs and the lipid nanoparticles that are ways that we could get to a better precision editing. These EDVs I guess
Note: This podcast is a companion to the Ground Truths newsletter “A Big Week for GLP-1 Drugs”Eric Topol (00:06):It is Eric Topol with Ground Truths, and with me today is Dr. Daniel Drucker from the University of Toronto, who is one of the leading endocrinologists in the world, and he along with Joel Habener and Jens Juul Holst from the University of Copenhagen and Denmark, have been credited with numerous prizes of their discovery work of glucagon-like peptide-1 (GLP-1) as we get to know these family of drugs and he's a true pioneer. He's been working on this for decades. So welcome, Daniel.Daniel Drucker (00:43):Thank you.Eric Topol (00:45):Yeah, it's great to have you and to get the perspective, one of the true pioneers in this field, because to say it's blossom would be an understatement, don't you think?Daniel Drucker (00:57):Yeah, it's been a bit of a hectic three years. We had a good quiet 30 plus years of solid science and then it's just exploded over the last few years.Eric Topol (01:06):Yeah, back in 30 years ago, did you have any sense that this was coming?Daniel Drucker (01:14):Not what we're experiencing today, I think there was a vision for the diabetes story. The first experiments were demonstrating insulin secretion and patents were followed around the use for the treatment of GLP-1 for diabetes. The food intake story was much more gradual and the weight loss story was quite slow. And in fact, as you know, we've had a GLP-1 drug approved for people with obesity since 2014, so it's 10 years since liraglutide was approved, but it didn't really catch the public's attention. The weight loss was good, but it wasn't as spectacular as what we're seeing today. So this really has taken off just over the last three, four years.Eric Topol (01:58):Yeah, no, it's actually, I've never seen a drug class like this in my life, Daniel. I mean, I've obviously witnessed the statins, but this one in terms of pleiotropy of having diverse effects, and I want to get to the brain here in just a minute because that seems to be quite a big factor. But one thing just before we get too deep into this, I think you have been great to recognize one of your colleagues who you work with at Harvard, Svetlana Mojsov. And the question I guess is over the years, as you said, there was a real kind of incremental path and I guess was in 1996 when you said, well, this drug likely will inhibit food intake, but then there were gaps of many years since then, as you mentioned about getting into the obesity side. Was that because there wasn't much weight loss in the people with diabetes or was it related to the dose of the drugs that were being tested?Why Did It Take So Long to Get to Obesity?Daniel Drucker (03:11):Well, really both. So the initial doses we tested for type 2 diabetes did not produce a lot of weight loss, maybe 2-3%. And then when we got semaglutide for type 2 diabetes, maybe we were getting 4-5% mean weight loss. And so that was really good and that was much better than we achieved before with any glucose lowering drug. But a lot of credit goes to Novo Nordisk because they looked at the dose for liraglutide and diabetes, which was 1.8 milligrams once daily for people with type 2 diabetes. And they asked a simple question, what if we increase the dose for weight loss? And the answer was, we get better weight loss with 3 milligrams once a day. So they learn that. And when they introduced semaglutide for type 2 diabetes, the doses were 0.5 and 1 milligrams. But in the back of their minds was the same question, what if we increased the dose and they landed on 2.4 milligrams once a week. And that's when we really started to see that the unexpected spectacular weight loss that we're now quite familiar with.Eric Topol (04:16):Was there also something too that diabetics don't lose as much weight if you were to have match dose?Daniel Drucker (04:22):Yeah, that's a general phenomenon. If one goes from either diet to bariatric surgery, and certainly with weight loss medicines, we tend to see maybe two thirds to three quarters of the amount of weight loss in people with type 2 diabetes. We don't really understand it. The brain pathways are probably resistant to some of the pathways that are activated that lead to weight loss, and it's really an interesting observation that needs further study.The Brain EffectEric Topol (04:50):Yeah, it's fascinating really. And it might've at least in part, held up this progress that has been truly remarkable. Now, recently you published a paper among many, you're a very prolific scientist, of course, physician scientist, but back in December in Cell Metabolism was a very important paper that explored the brain gut axis, the ability to inhibit inflammation and the mechanism through Toll-like receptors that you were seeing that. So maybe you could summarize the fact that you saw this, you were quoted in this Atlantic piece by Sarah Zhang, the science behind Ozempic was wrong. The weight loss effects of GLP-1 drugs have little to do with the gut and basically claiming that it's related to the effects on the brain, which of course could be reduced inflammation, reduced or inhibiting centers of addiction craving, that sort of thing. So how do you interpret your recent results and ongoing studies regarding GLP-1's effect on the brain?Daniel Drucker (06:02):Sure, so to be clear, I don't think that was a quote. I never would've said the science behind Ozempic was wrong. I think that was a headline writer doing what they do best, which is catching people's attention. I think what I was trying to say is that where this field started with insulin secretion first and then weight loss second, those are clearly very important pharmacological attributes of GLP-1. But physiologically, if we take GLP-1 away or we take the receptor away, you don't really develop diabetes without GLP-1. You don't really gain a lot of weight without GLP-1. So physiologically it's not that important. Why do we have GLP-1 in the distal gut? I think physiologically it's there to defend against infection and reduce gut inflammation. But we noticed that GLP-1 reduces inflammation in many different places in the heart and blood vessels and in the liver and many organs where you don't see a lot of GLP-1 receptors and you don't see a lot of GLP-1 receptors on immune cells.Daniel Drucker (07:04):So that really led us to the question, well, how does it work and affect all these organs where we don't see a lot of the receptors? And that's where we landed on the brain. Obviously the nervous system can communicate with many different cell types in almost every organ. And we identified neurons that expressed the GLP-1 receptor, which when blocked abrogated or completely eliminated the ability of GLP-1 to reduce inflammation in the periphery in white cells or in lungs. So it's been known for some time that the brain can control the immune system. So this is just the latest piece in the puzzle of how GLP-1 might reduce inflammation.Eric Topol (07:49):And just to be clear, I was quoting the Atlantic headline, not you that you were quoted within that article, but this is something that's really interesting because obviously GLP-1 is made in the brain in certain parts of the brain, it's transient in terms of its half-life made from the gut. But when we give these drugs, these agonists, how does it get in the brain? Because isn't there a problem with the blood brain barrier?Daniel Drucker (08:22):So I don't think the drugs get into the brain very well. We have a lot of data on this, so people have done the classic experiments, they either make radioactive ligands or fluorescent ligands, and they look how much gets in it and not very much gets in beyond the blood-brain barrier. And we also have big drugs that are immunoglobulin based and they work really well, so they don't get into the brain very much at all. And so, the way I describe this is that GLP-1 talks to the brain, but it doesn't directly get into the brain to meaningful extent, it does communicate somewhat there are areas obviously that are accessible in the area of the stream and circumventricular organs, but most of the time we have this communication that's not well understood that results in the magic that we see. And there are some discussions around for the neurodegenerative disease story where GLP-1 is being looked at in Parkinson's disease and in people with Alzheimer's disease. Would you be able to get more benefit if you could get the drugs into the brain to a greater extent, or would you simply increase the adverse event profile and the adverse response? So really important area for study as we begin to go beyond diabetes and obesity.Eric Topol (09:41):Yeah, I mean as you're pointing out, there's two ongoing trials, pretty large trials in Alzheimer's, early Alzheimer's, which may be a little bit too late, but at any rate, testing GLP-1 to see whether or not it could help prevent progression of the disease. And as you also mentioned, diseases and Parkinson's. But I guess, so the magic as you referred to it, the gut -brain axis so that when you give the GLP-1 family of drugs, we'll talk more about the double and triple receptor in a moment, but when you give these drugs, how does the message you get from the gut to the brain would you say?Daniel Drucker (10:27):So pharmacologically, we can give someone or an animal the drug, it does reach some of the accessible neurons that have GLP-1 receptors, and they probably transmit signals deeper into the brain and then activate signal transduction. So one way to look at it, if you use c-fos, the protein, which is an immediate early gene, which is increased when we activate neurons, we see rapid activation of c-fos in many regions that are deep within the brain within minutes. And we know that GLP-1 is not getting directly to those neurons, but it's activating pathways that turn on those neurons. And so, there's probably a very intricate set of p
Siddhartha Mukherjee is a Professor at Columbia University, oncologist, and extraordinary author of Emperor of All Maladies (which was awarded a Pulitzer Prize), The Gene, and The Song of the Cell, along with outstanding pieces in the New Yorker. He is one of the top thought leaders in medicine of our era. “I have begun to imagine, think about what it would be to be a digital human..”—Sid MukherjeeEric Topol (00:06):Well, hello, this is Eric Topol with Ground Truths, and I am delighted to have my friend Sid Mukherjee, to have a conversation about all sorts of interesting things. Sid, his most recent book, SONG OF THE CELL is extraordinary. And I understand, Sid, you're working on another book that may be cell related. Is that right?Sid Mukherjee (00:30):Eric, it's not cell related, I would say, but it's AI and death related, and it covers, broadly speaking, it covers AI, longevity and death and memory —topics that I think are universal, but also particularly medicine.Eric Topol (00:57):Well, good, and we'll get into that. I had somehow someone steered me that your next book was going to be something building on the last one, but that sounds even more interesting. You're going in another direction. You've covered cancer gene cells, so I think covering this new topic is of particularly interest. So let's get into the AI story and maybe we'll start off with your views on the healthcare side. Where do you think this is headed now?A.I. and Drug DiscoverySid Mukherjee (01:29):So I think Eric, there are two very broad ways of dividing where AI can enter healthcare, and there may be more, I'm just going to give you two, but there may be more. One is on what I would call the deep science aspect of it, and by that I mean AI-based drug discovery, AI-based antibody discovery, AI-based modeling. All of which use AI tools but are using tools that have to do with machine learning, but may have to do less directly with the kind of large language models. These tools have been in development for a long time. You and I are familiar with them. They are tools. Very simply put, you can imagine that the docking of a drug to a protein, so imagine every drug, every medicine as a small spaceship that docks onto a large spaceship, the large spaceship being the target.(02:57):So if you think of it that way, there are fundamental rules. If anyone's watched Star Wars or any of these sci-fi films, there are fundamental rules by which that govern the way that the small spaceship in this case, a molecule like aspirin fits into a pocket of its target, and those are principles that are determined entirely by chemistry and physics, but they can be taught, you can learn what kind of spaceship or molecule is likely to fit into what kind of pocket of the mothership, in this case, the target. And if they can be learned, they're amenable to AI-based discovery.Eric Topol (03:57):Right. Well, that's, isn't that what you'd call the fancy term structure-based discovery, where you're using such tools like what AlphaFold2 for proteins and then eventually for antibodies, small molecules, et cetera, that you can really rev up the whole discovery of new molecules, right?Sid Mukherjee (04:21):That's correct, and that's one of the efforts that I'm very heavily involved in. We have created proprietary algorithms that allow us to enable this. Ultimately, of course, there has to be a method by which you start from these AI based methods, then move to physical real chemistry, then move to real biology, then move to obviously human biology and ultimately to human studies. It's a long process, but it's an incredibly fruitful process.Eric Topol (04:57):Well, yeah, as an example that recently we had Jim Collins on the podcast and he talked about the first new drug class of antibiotics in two decades that bind to staph aureus methicillin resistant, and now in clinical trials. So it’s happening. There’s 20 AI drugs in clinical trials out there.Sid Mukherjee (05:18):It’s bound to happen. It is an unstoppable bound to happen systematology of drug discovery. This is just bound to happen. It is unstoppable. There are kinks in it in the road, but those will be ironed out, but it’s bound to happen.(05:41):So that’s on the very discovery oriented end, which is more related to learning algorithms that have to do with AI and less to do with what we see in day-to-day life, the ChatGPT kind of day-to-day life of the world. On the very other end of the spectrum, just to move along on the very other end of the spectrum are what I would call patient informatics. So by patient informatics, I mean questions like who responds to a particular drug? What genes do they have? What environment are they in? Have they had other drug interactions in the past? What is it about their medical record that will allow us to understand better why or why they're not responding to a medicine?(06:51):Those are also AI, can also be really powered by AI, but are much more dependent and much more sensitive to our understanding of these current models, the large language models. So just to give you an example, let's say you wanted to enroll a clinical trial for patients with diabetes to take a new drug. You could go into the electronic medical record, which right now is a text file, and ask the question, have they or have they not responded to the standard agents? And what has their response been? Should they be on glucose monitoring? How bad is their diabetes based on some laboratory parameters, et cetera, et cetera. So that's a very different information rich, electronic medical record rich mechanism to understand how to develop medicines. One lies, the first lies way in the discovery end of the spectrum. The second lies way in the clinical trials and human drug exposure end of the spectrum. And of course, there are things in the middle that I haven't iterated, but those are the two really broad categories where one can imagine AI making a difference and to be fair through various efforts, I'm working on both of those, the two end spectrum.A.I. and CancerEric Topol (08:34):Well, let's drill down a bit more on the person individual informatics for a moment, since you're an oncologist, and the way we screen for cancer today is completely ridiculous by age only. But if you had a person's genome sequence, polygenic risk scores for cancers and all the other known data that, for example, the integrity of their immune system response, environmental exposures, which we'll talk about in a moment more, wouldn't we do far better for being able to identify high risk people and even preventing cancer in the future?Sid Mukherjee (09:21):So I have no doubt whatsoever that more information that we can analyze using intelligent platforms. And I'm saying all of these words are relevant, more information analyzed through intelligent platforms. More information by itself is often useless. Intelligent platforms without information by themselves are often useless, but more information with intelligent platforms, that combination can be very useful. And so, one use case of that is just to give you one example, there are several patients, women who have a family history of breast cancer, but who have no mutations in the known single monogenic breast cancer risk genes, BRCA1, BRCA2, and a couple of others. Those patients can be at a high a risk of breast cancer as patients who have BRCA1 and BRCA2. It's just that their risk is spread out through not one gene but thousands of genes. And those patients, of course have to be monitored and their risk is high, and they need to understand what the risk is and how to manage it.(10:57):And that's where AI can, and first of all, informatics and then AI can play a big difference because we can understand how to manage those patients. They used to be called, this is kind of, I don't mean this lightly, but they used to be called BRCA3 because they didn't have BRCA1, they didn't have BRCA2, but they had a constellation of genes, not one, not two, but thousands of genes that would increase their risk of breast cancer just a little bit. I often describe these as nudge genes as opposed to shove genes. BRCA1 and BRCA2 are shoved genes. They shove you into having a high risk of breast cancer. But you can imagine that there are nudge genes as well in which they, in which a constellation of not one, not two, not three, but a thousand genetic variations, give a little push each one, a little push towards having a higher risk of breast cancer.(12:09):Now, the only way to find these nudge genes is by doing very clever informatic studies, some of which have been done in breast cancer, ovarian cancer, cardiovascular diseases, other diseases where you see these nudge effects, small effects of a single gene, but accumulated across a thousand, 2000, 3000 genes, an effect that's large enough that it's meaningful. And I think that we need to understand those. And once we understand them, I think we need to understand what to do with these patients. Do we screen them more assertively? Do we recommend therapies? You can get more aggressive, less aggressive, but of course that demands clinical trials and a deeper understanding of the biology of what happens.A.I. And LongevityEric Topol (13:10):Right, so your point about the cumulative effects of small variants, hundreds and hundreds of these variants being equivalent potentially, as we've seen across many diseases, it's really important and you're absolutely right about that. And I've been pushing for trying to get these polygenic risk scores into clinical routine use, and hopefully we're getting closer to that. And that's just as you say, just one layer of this information to add to the intelligence platform. Now, the next thing that you haven't yet touched on connecting the dots is, can AI and informatics be used to promote longevity?Sid Mukherjee (13:55):Yeah, so that's a very interesting question. Let me attack that question in two ways. One biological
There was so much to talk about—this is the longest Ground Truths podcast yet. Hope you’ll find it as thought-provoking as I did!Transcript, with audio and external links, edited by Jessica Nguyen, Producer for Ground TruthsVideo and audio tech support by Sinjun Balabanoff, Scripps ResearchEric Topol (00:00:05):This is Eric Topol from Ground Truths, and I am delighted to have with me Holden Thorp, who is the Editor-in-Chief of the Science journals. We're going to talk about Science, not just the magazine journal, but also science in general. This is especially appropriate today because Holden was just recognized by STAT as one of the leaders for 2024 because of his extraordinary efforts to promote science integrity, so welcome Holden.Holden Thorp (00:00:36):Thanks Eric, and if I remember correctly, you were recognized by STAT in 2022, so it's an honor to join a group that you're in anytime, that's for sure, and great to be on here with you.Eric Topol (00:00:47):Well, that's really kind to you. Let's start off, I think with the journal, because I know that consumes a lot of your efforts and you have five journals within science.Holden Thorp (00:01:02):Oh, we have six.Eric Topol (00:01:03):Oh six, I'm sorry, six. There's Science, the original, and then five others. Can you tell us what it's like to oversee all these journals?Overseeing the Science JournalsHolden Thorp (00:01:16):Yeah, we're a relatively small family compared to our commercial competitors. I know you had Magdalena [Skipper]on and Nature has I think almost ninety journals, so six is pretty small. In addition to Science, which most people are familiar with, we have Science Advances, which also covers all areas of science and is larger and is a gold open access journal and also is overseen by academic editors, not professional editors. All of our other journals are overseen by professional editors. And then the other four are relatively small and specialized areas, and probably people who listen to you and follow you would know about Science Translational Medicine, Science Immunology, Science Signaling and then we also have a journal, Science Robotics which is something I knew nothing about and I learned a lot. I've learned a lot about robotics and the culture of people who work there interacting with them.Holden Thorp (00:02:22):So we have a relatively small family. There's only 160 people who work for me, which is manageable. I mean that sounds like a lot, but in my previous jobs I was a provost and a chancellor, and I had tens of thousands of people, so it's really fun for me to have a group where I at least have met everybody who works for me. We're an outstanding set of journals, so we attract an outstanding group of professionals who do all the things that are involved in all this, and it's really, really fun to work with them. At Science, we don't just do research papers, although that's a big, and probably for your listeners the biggest part of what we do. But we also have a news and commentary section and the news section is 30 full-time and many freelancers around the world really running the biggest general news operation for science that there is. And then in the commentary section, which you're a regular contributor for us in expert voices, we attempt to be the best place in the world for scientists to talk to each other. All three of those missions are just really, really fun for me. It's the best job I've ever had, and it's one I hope to do for many years into the future.Eric Topol (00:03:55):Well, it's extraordinary because in the four and a half years I think it's been since you took the helm, you've changed the face of Science in many ways. Of course, I think the other distinction from the Nature Journals is that it's a nonprofit entity, which shows it isn't like you're trying to proliferate to all sorts of added journals, but in addition, what you've done, at least the science advisor and the science news and all these things that come out on a daily basis is quite extraordinary as we saw throughout the pandemic. I mean, just reporting that was unparalleled from, as you say, all points around the world about really critically relevant topics. Obviously it extends well beyond the concerns of the pandemic. It has a lot of different functions, but what I think you have done two major things, Holden. One is you medicalized it to some extent.Eric Topol (00:04:55):A lot of people saw the journal, particularly Science per se, as a truly basic science journal. Not so much applied in a medical sphere, but these days there's more and more that would be particularly relevant to the practice of medicine, so that's one thing. And the other thing I wanted you to comment on is you're not afraid to speak out and as opposed to many other prior editors who I followed throughout my career at Science, there were pretty much the politically correct type and they weren't going to really express themselves, which you are particularly not afraid of. Maybe you could comment about if you do perceive this medicalization of science to some extent, and also your sense of being able to express yourself freely.Capturing the Breakthroughs in Structural BiologyHolden Thorp (00:05:48):Yeah, well, you're kind to say both of those things are certainly things we have worked at. I mean, I do come from a background, even though I'm trained as a chemist, most of what I did towards the latter end of my career, I mean, I did very basic biochemistry when I was a researcher, but the last part of my research career I worked in on development of a drug called Vivjoa, which is an alternative to the fluconazole family that doesn't have the same toxicity and is currently on the market for chronic yeast infection and hopefully some other things in the future when we can get some more clinical trials done.Holden Thorp (00:06:35):And I've hung around biotech startups and drug development, so it is part of the business that I knew. I think the pandemic really gave us an opening because Valda Vinson, who's now the Executive Editor and runs all of life sciences for us and policies for the journal, she was so well known in structural biology that most of the first important structures in Covid, including the spike protein, all came to us. I mean, I remember crystal clear February of 2020, she came in my office and she said, I got the structure of the spike protein. And I said, great, what's the spike protein? Turned out later became the most famous protein in the world, at least temporarily. Insulin may be back to being the most famous protein now, but spike protein was up there. And then that kind of cascaded into all the main protease and many of the structures that we got.Holden Thorp (00:07:45):And we seized on that for sure, to kind of broaden our focus. We had the Regeneron antibodies, we had the Paxlovid paper, and all of that kind of opened doors for us. And we've also, now we have two clinical editors at Science, Priscilla Kelly and Yevgeniya Nusinovich, and then the Insights section, somebody that you work with closely, Gemma Alderton, she is very fluent in clinical matters. And then of course we've had Science Translational Medicine and we seek continue to strengthen that. Science Immunology was very much boosted by Covid and actually Science Immunology is now, I think probably if you care about impact factors, the second highest specialized immunology journal after Immunity. I've put some emphasis on it for sure, but I think the pandemic also really helped us. As far as me speaking out, a lot of people maybe don't remember, but Don Kennedy, who was the editor in the early 2000s who had been the Stanford president, he was similarly outspoken.Confronting ControversiesHolden Thorp (00:09:15):It's funny, sometimes people who disagree with me say, well, Don Kennedy would never say anything like that. And then I can dig up something that Don Kennedy said that's just as aggressive as what I might've said. But you're right, Bruce Alberts was very focused on education, and each one of us has had our own different way of doing things. When Alan Leshner hired me and Sudip Parikh reinforced this when he came on, I mean, he wanted me to liven up the editorial page. He explicitly told me to do that. I may have done more of it than he was expecting, but Alan and Sudip both still remain very supportive of that. I couldn't do what I do without them and also couldn't do it without Lisa Chong, who makes all my words sound so much better than they are when I start. And yeah, it kind of fed on itself.Holden Thorp (00:10:21):It started with the pandemic. I think there was an inflection when Trump first said that Covid was just the flu, and when he said some really ridiculous things about the vaccine, and that's where it started. I guess my philosophy was I was thinking about people who, they've got a spouse at home whose job might be disrupted. They got children they've got who are out of school, and somehow they managed to get themselves to the lab to work on our vaccine or some other aspect of the pandemic to try to help the world. What would those people want their journal to say when they came home and turned the news on and saw all these politicians saying all this ridiculous stuff? That was really the sort of mantra that I had in my head, and that kind of drove it. And now I think we've sort of established the fact that it's okay to comment on things that are going on in the world. We're editorially independent, Sudip and the AAAS board, treat us as being editorially independent. I don't take that for granted and it's a privilege to, as I sometimes tell people, my apartment's four blocks from the White House, sometimes I'm over there typing things that they don't like. And that tradition is still alive in this country, at least for the time being, and I try to make the most of it.Eric Topol (00:12:11):Well, and especially as you already touched on Holden, when there's a time when the inte
Transcript Eric Topol (00:06):Well, hello, this is Eric Topol with Ground Truths and I am absolutely thrilled to welcome Daphne Koller, the founder and CEO of insitro, and a person who I've been wanting to meet for some time. Finally, we converged so welcome, Daphne.Daphne Koller (00:21):Thank you Eric. And it's a pleasure to finally meet you as well.Eric Topol (00:24):Yeah, I mean you have been rocking everybody over the years with elected to the National Academy of Engineering and Science and right at the interface of life science and computer science and in my view, there's hardly anyone I can imagine who's doing so much at that interface. I wanted to first start with your meeting in Davos last month because I kind of figured we start broad AI rather than starting to get into what you're doing these days. And you had a really interesting panel [←transcript] with Yann LeCun, Andrew Ng and Kai-Fu Lee and others, and I wanted to get your impression about that and also kind of the general sense. I mean AI is just moving it at speed, that is just crazy stuff. What were your thoughts about that panel just last month, where are we?Video link for the WEF PanelDaphne Koller (01:25):I think we've been living on an exponential curve for multiple decades and the thing about exponential curves is they are very misleading things. In the early stages people basically take the line between whatever we were last year, and this year and they interpolate linearly, and they say, God, things are moving so slowly. Then as the exponential curve starts to pick up, it becomes more and more evident that things are moving faster, but it’s still people interpolate linearly and it's only when things really hit that inflection point that people realize that even with the linear interpolation where we'll be next year is just mind blowing. And if you realize that you're on that exponential curve where we will be next year is just totally unanticipatable. I think what we started to discuss in that panel was, are we in fact on an exponential curve? What are the rate limiting factors that may or may not enable that curve to continue specifically availability of data and what it would take to make that curve available in areas outside of the speech, whatever natural language, large language models that exist today and go far beyond that, which is what you would need to have these be applicable to areas such as biology and medicine.Daphne Koller (02:47):And so that was kind of the message to my mind from the panel.Eric Topol (02:53):And there was some differences in opinion, of course Yann can be a little strong and I think it was good to see that you're challenging on some things and how there is this “world view” of AI and how, I guess where we go from here. As you mentioned in the area of life science, there already had been before large language models hit stride, so much progress particularly in imaging cells, subcellular, I mean rare cells, I mean just stuff that was just without any labeling, without fluorescein, just amazing stuff. And then now it's gone into another level. So as we get into that, just before I do that, I want to ask you about this convergence story. Jensen Huang, I'm sure you heard his quote about biology as the opportunity to be engineering, not science. I'm sure if I understand, not science, but what about this convergence? Because it is quite extraordinary to see two fields coming together moving at such high velocity."Biology has the opportunity to be engineering not science. When something becomes engineering not science it becomes...exponentially improving, it can compound on the benefits of previous years." -Jensen Huang, NVIDIA.Daphne Koller (04:08):So, a quote that I will replace Jensen's or will propose a replacement for Jensen's quote, which is one that many people have articulated, is that math is to physics as machine learning is to biology. It is a mathematical foundation that allows you to take something that up until that point had been kind of mysterious and fuzzy and almost magical and create a formal foundation for it. Now physics, especially Newtonian physics, is simple enough that math is the right foundation to capture what goes on in a lot of physics. Biology as an evolved natural system is so complex that you can't articulate a mathematical model for that de novo. You need to actually let the data speak and then let machine learning find the patterns in those data and really help us create a predictability, if you will, for biological systems that you can start to ask what if questions, what would happen if we perturb the system in this way?The ConvergenceDaphne Koller (05:17):How would it react? We're nowhere close to being able to answer those questions reliably today, but as you feed a machine learning system more and more data, hopefully it'll become capable of making those predictions. And in order to do that, and this is where it comes to this convergence of these two disciplines, the fodder, the foundation for all of machine learning is having enough data to feed the beast. The miracle of the convergence that we're seeing is that over the last 10, 15 years, maybe 20 years in biology, we've been on a similar, albeit somewhat slower exponential curve of data generation in biology where we are turning it into a quantitative discipline from something that is entirely observational qualitative, which is where it started, to something that becomes much more quantitative and broad based in how we measure biology. And so those measurements, the tools that life scientists and bioengineers have developed that allow us to measure biological systems is what produces that fodder, that energy that you can then feed into the machine learning models so that they can start making predictions.Eric Topol (06:32):Yeah, well I think the number of layers of data no less what's in these layers is quite extraordinary. So some years ago when all the single cell sequencing was started, I said, well, that's kind of academic interest and now the field of spatial omics has exploded. And I wonder how you see the feeding the beast here. It's at every level. It's not just the cell level subcellular and single cell nuclei sequencing single cell epigenomics, and then you go all the way to these other layers of data. I know you plug into the human patient side as well as it could be images, it could be past slides, it could be the outcomes and treatments and on and on and on. I mean, so when you think about multimodal AI, has anybody really done that yet?Daphne Koller (07:30):I think that there are certainly beginnings of multimodal AI and we have started to see some of the benefits of the convergence of say, imaging and omics. And I will give an example from some of the work that we've recently distributed on a preprint server work that we did at insitro, which took imaging data from standard histopathology slides, H&E slides and aligned them with simple bulk RNA-Seq taken from those same tumor samples. And what we find is that by training models that translate from one to the other, specifically from the imaging to the omics, you're able to, for a fairly large fraction of genes, make very accurate predictions of gene expression levels by looking at the histopath images alone. And in fact, because many of the predictions are made at the tile level, not at the entire slide level, even though the omics was captured in bulk, you're able to spatially resolve the signal and get kind of like a pseudo spatial biology just by making predictions from the H&E image into these omic modalities.Multimodal A.I. and Life ScienceDaphne Koller (08:44):So there are I think beginnings of multimodality, but in order to get to multimodality, you really need to train on at least some data where the two modalities are simultaneously. And so at this point, I think the rate limiting factor is more a matter of data acquisition for training the models. It is for building the models themselves. And so that's where I think things like spatial biology, which I think like you are very excited about, are one of the places where we can really start to capture these paired modalities and get to some of those multimodal capabilities.Eric Topol (09:23):Yeah, I wanted to ask you because I mean spatial temporal is so perfect. It is two modes, and you have as the preprint you refer to and you see things like electronic health records in genomics, electronic health records in medical images. The most we've done is getting two modes of data together. And the question is as this data starts to really accrue, do we need new models to work with it or do you actually foresee that that is not a limiting step?Daphne Koller (09:57):So I think currently data availability is the most significant rate limiting step. The nice thing about modern day machine learning is that it really is structured as a set of building blocks that you can start to put together in different ways for different situations. And so, do we have the exact right models available to us today for these multimodal systems? Probably not, but do we have the right building blocks that if we creatively put them together from what has already been deployed in other settings? Probably, yes. So of course there's still a model exploration to be done and a lot of creativity in how these building blocks should be put together, but I think we have the tools available to solve these problems. What we really need is first I think a really significant data acquisition effort. And the other thing that we need, which is also something that has been a priority for us at insitro, is the right mix of people to be put together so that you can, because what happens is if you take a bunch of even extremely talented and sophisticated machine learning scientists and say, solve a biological problem, here's a dataset, they don't know what questions to ask and oftentimes end up asking questions that might be kind of interestin
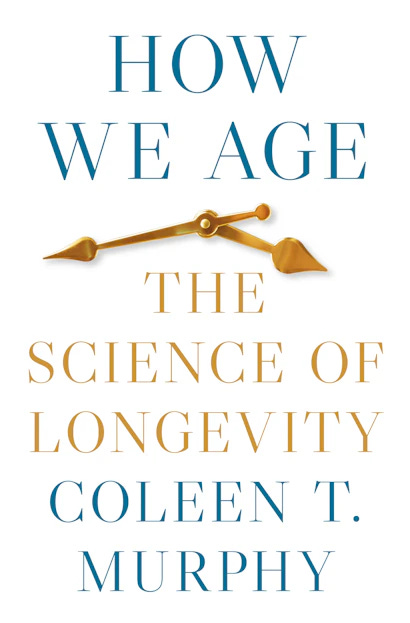
“A few years ago, I might have chuckled at the naiveté of this question, but now it's not so crazy to think that we will be able to take some sort of medicine to extend our healthy lifespans in the foreseeable future.”—Coleen MurphyTranscript with external linksEric Topol (00:06):Hello, this is Eric Topol from Ground Truths, and I'm just so delighted to have with me Professor Coleen Murphy, who has written this exceptional book, How We Age: The Science of Longevity. It is a phenomenal book and I'm very eager to discuss it with you, Coleen.Coleen Murphy (00:25):Thanks for having me on.Eric Topol (00:27):Oh yeah. Well, just so everyone who doesn't know Professor Murphy, she's at Princeton. She's the Richard Fisher Preceptor in Integrative Genomics, the Lewis-Sigler Institute for Integrative Genomics at Princeton, and director of the Paul Glenn Laboratories for Aging Research. Well, obviously you've been in this field for decades now, even though you're still very young. The classic paper that I can go back to would be in Nature 2003 with the DAF-16 and doubling the lifespan of C. elegans or better known as a roundworm. Would that be the first major entry you had?Coleen Murphy (01:17):Yeah, that was my postdoctoral work with Cynthia Kenyon.Eric Topol (01:20):Right, and you haven't stopped since you've been on a tear and you’ve put together a book which has a hundred pages of references in a small font. I don't know what the total number is, but it must be a thousand or something.Coleen Murphy (01:35):Actually, it's just under a thousand. That's right.Eric Topol (01:37):That's a good guess.Coleen Murphy (01:38):Good guess. Yeah.Eric Topol (01:39):So, because I too have a great interest in this area, I found just the resource that you've put together as extraordinary in terms of the science and all the work you've put together. What I was hoping to do today is to kind of take us through some of the real exciting pathways because there's a sentence in your book, which I thought was really kind of nailed it, and it actually is aligned with my sense. Obviously don't have the expertise by any means that you do here but it says, “A few years ago, I might have chuckled at the naivety of this question, but now it's not so crazy to think that we will be able to take some sort of medicine to extend our healthy lifespans in the foreseeable future.” That's a pretty strong statement for a person who's deep into the science. First I thought we'd explore healthy aging health span versus lifespan. Can you differentiate that as to your expectations?Coleen Murphy (02:54):So, I think most people would agree that they don't want to live necessary super long. What they really want to do is live a healthy life as long as they can. I think that a lot of people also have this fear that when we talk about extending lifespan, that we're ignoring that part. And I do want to assure everyone that the people in the researchers in the aging field are very much aware of this issue and have, especially in the past decade, I think put a real emphasis on this idea of quality of life and health span. What's reassuring is actually that many of the mechanisms that extend lifespan in all these model organisms also extend health span as well and so I don't think we're going to, they're not diametrically opposed, like we'll get to a healthier quality of life, I think in these efforts to extend lifespan as well.Eric Topol (03:50):Yeah, I think that's important that you're bringing that up, which is there's this overlap, like a Venn diagram where things that do help with longevity should help with health span, and we don't necessarily have to follow as you call them the immoralists, as far as living to 190 or whatever year. Now, one of the pathways that's been of course a big one for years and studied in multiple species has been caloric restriction. I wonder if you could talk to that and obviously there's now mimetics that could simulate that so you wouldn't have to go through some major dietary starvation, if you will. What are your thoughts on that pathway?Coleen Murphy (04:41):Yeah, actually I'm really glad you brought up mimetics because often the conversation starts and ends with you should eat less. I think that is a really hard thing for a lot of people to do. So just for the background, so dietary restriction or caloric restriction, the idea is that you would have to take in up to 30% less than your normal intake in order to start seeing results. When we've done this with laboratory animals of all kinds, this works from yeast all the way up through mice, actually primates, in fact, it does extend lifespan and in most metrics of health span the quality of life, it does improve that as well. On the other hand, I think psychologically it's really tough to not eat enough and I think that's a part that we kind of blindly ignore when we talk about this pathway.Coleen Murphy (05:30):And of course, if we gave any of those animals the choice of whether they want to start eating more, they would. So, it's like that's not the experiment we ever hear about. And so, the idea for studying this pathway isn't just to say, okay, this works and now we know how it works, but as you pointed out, mimetics, so can we target the molecules in the pathway so that we can help people achieve the benefits of caloric restriction without necessarily having to do the kind of awful part of restriction? I think that's really cool, and especially it might be very good for people who are undergoing certain, have certain diseases or have certain impairments that it might make it difficult ever to do dietary restrictions, so I think that's a really great thing that the field is kind of getting towards now.Eric Topol (06:15):And I think in fact, just today, it's every day there's something published now. Just today there was a University of Southern California study, a randomized study report comparing plant-based fasting-mimicking diet versus controlled diet, and showed that many metabolic features were improved quite substantially and projected that if you stayed on that diet, you'd gain two and a half years of healthy aging or that you would have, that's a bit of an extrapolation, but quite a bit of benefit. Now, what candidates would simulate caloric restriction? I mean, what kind of molecules would help us do that? And by the way, in the book you mentioned that the price to pay is that the brain slows down with caloric restrictions.Coleen Murphy (07:10):There's at least one study that shows that.Coleen Murphy (07:13):Yeah, so it's good to keep in mind. One of the big things that is being looked at as rapamycin, looking at that TOR pathway. So that's being explored as one of these really good mimetics. And of course, you have things that are analogs of that, so rapalogs, and so people are trying to develop drugs that mimic that, do the same kind of thing without probably some of the side effects that you might see with rapamycin. Metformin is another one, although it's interesting when you talk to people about metformin who work on it, it's argued about what is exactly the target of metformin. There's thought maybe also acts in the TOR pathway could affect complex one of mitochondria. Some of the things we know that they work, and we don't necessarily know how they work. And then of course there's new drugs all the time where people are trying to develop to other target, other molecules. So, we'll see, but I think that the idea of mimetics is actually really good, and that part of the field is moving forward pretty quickly. This diet that you did just mention, it is really encouraging that they don't have to take a drug if you don't want to. If you eat the right kind of diet, it could be very beneficial.Eric Topol (08:20):Yeah, no, it was interesting. I was looking at the methods in that USC paper and they sent them a box of stuff that they would eat for three cycles, multiple weeks per cycle. It was a very interesting report, we'll link to that. Before we leave the caloric restriction and these mTOR pathway, you noted in the book that there some ongoing trials like PEARL, I looked that up and they finished the trial, but they haven't reported it and it's not that large. And then there's the FAME trial with metformin. I guess we'll get a readout on these trials in the not-too-distant future. Right?Coleen Murphy (08:57):Yeah, that's the hope that especially with the Metformin trial, which I think is going to be really large the FAME trial, that just to give the listeners a little background, one of the efforts in the field is not just to show that something works, but also to convince the FDA that aging could be a pharmaceutical, a disease that we might want to have interventions for. And to do that, we need to figure out the right way to do it. We can't do 30-year studies of safety and things to make sure that something's good, but maybe there are reasonable biomarkers that would tell us whether people are going to live a long time. And so, if we can use some of those things or targeting age-related diseases where we can get a faster readout as well. Those are reasonable things that companies could do that would help us to really confirm or maybe rule out some of these pharmaceuticals as effective interventions. I think that would be really great for consumers to know, is this thing really going to do good or not? And we just don't have that right now in the field. We have a lot of people saying something will work and it might and the studies in the lab, but when we get to humans, we really need more clinical studies to really tell us that things are going to be effective.Eric Topol (10:12):Right, I'm going to get to that in a bit too because I think you're bringing up a critical topic since there's an explosion of biopharma companies in this space, billions of dollars that have been put up for in capital and the question is what's going to be the ground rules to get these poten
Transcript with audio and relevant external links, recorded on 6 Feb 2024Eric Topol (00:05):Hello, this is Eric Topol with Ground Truths, and I have a remarkable guest with me today, Professor Michelle Monje, who is from Stanford, a physician-scientist there and is really a leader in neuro-oncology, the big field of cancer neuroscience, neuroinflammation, and she has just been rocking it recently with major papers on these fields, no less her work that's been on a particular cancer, brain cancer in kids that we'll talk about. I just want to give you a bit of background about Michelle. She is a National Academy of Medicine member, no less actually a National Academy of Medicine awardee with the French Academy for the Richard Lounsbery Award, which is incredibly prestigious. She received a Genius grant from the MacArthur Foundation and is a Howard Hughes Medical Institute (HHMI) scholar, so she is just an amazing person who I'm meeting for the first time. Michelle, welcome.Michelle Monje (01:16):Thank you. So nice to join you.Long Covid and the BrainEric Topol (01:18):Well, I just am blown away by the work that you and your colleagues have been doing and it transcends many different areas that are of utmost importance. Maybe we can start with Long Covid because that's obviously such a big area. Not only have you done work on that, but you published an amazing review with Akiko Iwasaki, a friend of mine, that really went through all the features of Long Covid. Can you summarize your thoughts about that?Michelle Monje (01:49):Yeah, and specifically we focused on the neurobiology of Long Covid focusing on the really common syndrome of cognitive impairment so-called brain fog after Covid even after relatively mild Covid. There has been this, I think really important and exciting, really explosion of work in the last few years internationally trying to understand this in ways that I am hopeful will be beneficial to many other diseases of cognition that occur in the context of other kinds of infections and other kinds of immune challenges. But what is emerging from our work and from others is that inflammation, even if it doesn't directly initially involve the nervous system, can very profoundly affect the nervous system and the mechanisms by which that can happen are diverse. One common mechanism appears to be immune challenge induced reactivity of an innate immune cell in the nervous system called microglia. These microglia, they populate the nervous system very early in embryonic development.(02:58):And their job is to protect the nervous system from infection, but also to respond to other kinds of toxic and infectious and immune challenges. They also play in healthy conditions, really important roles in neurodevelopment and in neuroplasticity and so they're multifaceted cells and this is some population of those cells, particularly in the white matter in the axon tracks that are exquisitely sensitive it seems to various kinds of immune challenges. So even if there's not a direct nervous system insult, they can react and when they react, they stop doing their normal helpful jobs and can dysregulate really important interactions between other kinds of cells in the brain like neurons and support cells for those neurons like oligodendrocytes and astrocytes. One common emerging principle is that microglial reactivity triggered by even relatively mild Covid occurring in the respiratory system, not directly infecting the brain or other kinds of immune challenges can trigger this reactivity of microglia and consequently dysregulate the normal interactions between cells and the brain.(04:13):So important for well-tuned and optimal nervous system function. The end product of that is dysfunction and cognition and kind of a brain fog impairment, attention, memory, ability to multitask, impaired speed of information processing, but there are other ways that Covid can influence the nervous system. Of course there can be direct infection. We don't think that that happens in every case. It may not happen even commonly, but it certainly can happen. There is a clear dysregulation of the vasculature, the immune response, and the reaction to the spike protein of Covid in particular can have very important effects on the vessels in the nervous system and that can trigger a cascade of effects that can cause nervous system dysregulation and may feed directly into that reactivity of the microglia. There also can be reactivation of other infections previous, for example, herpes virus infections. EBV for example, can be reactivated and trigger a new immune challenge in the context of the immune dysregulation that Covid can induce.(05:21):There also can be autoimmunity. There are many, we're learning all the different ways Covid can affect the nervous system, but autoimmunity, there can be mimicry of some of the antigens that Covid presents and unfortunate autoimmunity against nervous system targets. Then finally in severe Covid where there is cardiopulmonary compromise, where there is hypoxia and multi-organ damage, there can be multifaceted effects on the nervous system in severe disease. So many different ways, and probably that is not a comprehensive list. It is certainly not a mutually exclusive list. Many of these interactions can happen at the same time in the same individual and in different combinations but we're beginning to wrap our arms around all the different ways that Covid can influence the nervous system and cause this fairly consistent syndrome of impaired attention, memory, multitasking, and executive functions.Homology with Chemo BrainEric Topol (06:23):Yeah, well there's a lot there that you just summarized and particularly you highlighted the type of glia, the microglia that appear to be potentially central at least a part of the story. You also made analogy to what you've seen with chemotherapy, chemo brain. Maybe you could elaborate on that.Michelle Monje (06:42):Yeah, absolutely. So I've been studying the cognitive impairment that can happen after cancer therapies including chemotherapy, but also radiation and immunotherapy. Each time we develop a new model and dig in to understand what's going on and how these cancer therapies influence the nervous system, microglia emerge as sort of the unifying principle, microglial reactivity, and the consequences of that reactivity on other cell types within the nervous system. And so, understanding that microglia and their reactive state to toxic or immune challenges was central to chemotherapy induced cognitive impairment, at least in preclinical models in the laboratory and confirm by human tissue studies. I worried at the very beginning of the pandemic that we might begin to see something that looks a lot like chemotherapy induced cognitive impairment, this syndrome that is characterized by impaired attention, memory, executive function, speed of information processing and multitasking. When just a few months into the pandemic, people began to flood neurologists’ office complaining of exactly this syndrome. I felt that we needed to study it and so that was the beginning of what has become a really wonderful collaboration with Akiko Iwasaki. I reached out to her, kind of cold called her in the midst of the deep Covid shutdown and in 2020 and said, hey, I have this idea, would you like to work with me? She's as you know, just a thought leader in Covid biology and she's been an incredibly wonderful and valuable collaborator along the way in this.Eric Topol (08:19):Well, the two of you pairing up is kind of, wow, that's a powerful combination, no question. Now, I guess the other thing I wanted to get at is there've been many other studies that have been looking at Long Covid, how it affects the brain. The one that's frequently cited of course is the UK Biobank where they had CT or MRI scans before in people fortunately, and then once they had Covid or didn't get Covid and it had a lot of worrisome findings including atrophy and then there are others that in terms of this niche of where immune cells can be in the meninges, in the bone marrow or the skull of the brain. Could you comment on both those issues because they've been kind of coming back to haunt us in terms of the more serious potential effects of Covid on the brain?Michelle Monje (09:20):Yeah, absolutely and I will say that I think all of the studies are actually quite parsimonious. They all really kind of point towards the same biology, examining it at different levels. And so that UK Biobank study was so powerful because in what other context would someone have MRI scans across the population and cognitive testing prior to the Covid pandemic and then have paired same individual tests after a range of severity of Covid infection so it was just an incredibly important data set with control individuals in the same cohort of people. This longitudinal study has continued to inform us in such important ways and that study found that there were multiple findings. One is that there appears to be a small but significant atrophy in the neocortex. Two that there are also abnormalities in major white matter tracts, and three, that there is particular pathology within the olfactory system.(10:30):And we know that Covid induces as a very common early symptom, this loss of smell. Then together with those structural findings on MRI scans that individuals even with relatively mild acute disease, exhibited long-term deficits in cognitive function. That fits with some beautiful epidemiological studies that have been done across many thousands of individuals in multiple different geographic populations. Underscoring this consistent finding that Covid can induce lasting cognitive changes and as we begin to understand that biology, it fits with those structural changes that are observed. We do know that the olfactory system is particularly affected and so it makes sense that the olfactory system, which show those structural changes, the
Jim Collins is one of the leading biomedical engineers in the world. He’s been elected to all 3 National Academies (Engineering, Science, and Medicine) and is one of the founders of the field of synthetic biology. In this conversation, we reviewed the seminal discoveries that he and his colleagues are making at the Antibiotics-AI Project at MIT.Recorded 5 February 2024, transcript below with audio links and external links to recent publicationsEric Topol (00:05):Hello, it's Eric Topol with Ground Truths, and I have got an extraordinary guest with me today, Jim Collins, who's the Termeer Professor of Medical Engineering at MIT. He also holds appointments at the Wyss Institute and the Broad Institute. He is a biomedical engineer who's been making exceptional contributions and has been on a tear lately, especially in the work of discovery of very promising, exciting developments in antibiotics. So welcome, Jim.Jim Collins (00:42):Eric, thanks for having me on the podcast.Eric Topol (00:44):Well, this was a shock when I saw your paper in Nature in December about a new structure class of antibiotics, the one from 1962 to 2000. It took 38 years, and then there was another one that took 24 years yours, the structural antibiotics. Before I get to that though, I want to go back just a few years to the work you did published in Cell with halicin, and can you tell us about this? Because when I started to realize what you've been doing, what you've been chipping away here, this was a drug you found, halicin, as I can try to understand, it works against tuberculosis, c. difficile, enterobacter that are resistant, acinetobacter that are resistant. I mean, this is, and this is of course in mice models. Can you tell us how did you make that discovery before we get into I guess what's called the Audacious Project?Jim Collins (01:48):Yeah, sure. It's actually a fun story, so it is origins go broadly to institute wide event at MIT, so MIT in 2018 launched a major campus-wide effort focused on artificial intelligence. The institute, which had played a major role in the first wave of AI in the 1950s, 1960s, and a major wave in the second wave in the 1980s found itself kind of at the wheel in this third wave involving big data and deep learning and looked to correct that and to correct it the institute had a symposium and I had the opportunity to sit next to Regina Barzilay, one of our faculty here at MIT who specializes in AI and particularly AI applied to biomedicine and we really hit it off and realized we had interest in applying AI to drug discovery. My lab had focused on antibiotics to then close to 15 years, but primarily we're using machine learning and network biology to understand the mechanism of action of antibiotics and how resistance arise with the goal of boosting what we already had, with Regina we saw there was an opportunity to see if we could use deep learning to get after discovery.(02:55):And notably, as you kind of alluded in your introduction, there's really been a discovery void and the golden age of discovery antibiotics was in the forties, fifties and sixties before I was born and before you had the genomic revolution, the biotech revolution, AI revolution. Anyways, we got together with our two groups, and it was an unfunded project and we kind of cobbled together very small training set of 2,500 compounds that included 1,700 FDA approved drugs and 800 natural compounds. In 2018, 2019, when you started this, if you asked any AI expert should you initiate that study, they would say absolutely not, there's going to be two big data. The idea of these models are very data hungry. You need a million pictures of a dog, a million pictures of a cat to train a model to differentiate between the cat and the dog, but we ignored the naysayers and said, okay, let's see what we can do.(03:41):And we apply these to E. coli, so a model pathogen that's used in labs but is also underlies urinary tract infections. So it’s a look to see which of the molecules inhibited growth of the bacteria as evidence for antibacterial activity and we could have measured and we quantified each of their effects, but because we had so few compounds, we just discretized instead, if you inhibited at least 80% of the growth you were antibacterial, and if you didn't achieve that, you weren't antibacterial zero in ones. We then took the structure of each molecule and trained a deep learning model, specifically a graphical neural net that could look at those structures, bond by bond, substructure by substructure associated with whatever features you look to train with. In our case, making for good antibiotic, not for good antibiotic. We then took the train model and applied it to a drug repurposing hub as part of the Broad Institute that consists of 6,100 molecules in various stages of development as a new drug.(04:40):And we asked the model to identify molecules that can make for a good antibiotic but didn't look like existing antibiotics. So part of the discovery void has been linked to this rediscovery issue we have where we just keep discovering quinolones like Cipro or beta-lactams like penicillin. Well, anyways, from those criteria as well as a small tox model, only one molecule came out of that, and that was this molecule we called halicin, which was named after HAL, the killing AI computer system from 2001 Space Odyssey. In this case, we don't want it to kill humans, we want it to kill bacteria and as you alluded, it turned out to be a remarkably potent novel antibiotic that killed off multi-drug resistant extensively drugs, a pan-resistant bacteria went after to infections. It was affected against TB, it was affected against C. diff and acinetobacter baumannii and acted to a completely new mechanism of action.(05:33):And so we were very excited to see how AI could open up possibilities and enable one to explore chemical spaces in new and different ways. We took them model, then applied it to a very large chemical library of 1.5 billion molecules, looked at a subset of about 110 million that would be impossible for any grad student, any lab really to look at that experimentally but we looked at it in a model computer system and in three days could screen those 110 million molecules and identified several new additional candidates, one which we call salicin, which is the cousin of halicin that similes broad spectrum and acts to a novel mechanism of action.Eric Topol (06:07):So before we go further with this initial burst of discovery, for those who are not used to deep neural networks, I think most now are used to the convolutional neural network for images, but what you use specifically here as you alluded to, were graph neural networks that you could actually study the binding properties. Can you just elaborate a little bit more about these GNN so that people know this is one of the tools that you used?Jim Collins (06:40):Yeah, so in this case, the underlying structure of the model can actually represent and capture a graphical structure of a molecule or it might be of a network so that the underlying structure itself of the model will also look at things like a carbon atom connects to an oxygen atom. The oxygen atom connects to a nitrogen atom and so when you think back to the chemical structures we learned in high school, maybe we learned in college, if we took chemistry class in college, it was actually a model that can capture the chemical structure representation and begin to look at sub aspects of it, associating different properties of it. In this case, again, ours was antibacterial, but it could be toxic, whether it's toxic against a human cell and the model, the train model, the graph neural model can now look at new structures that you input them and then make calculations on those bonds so a bond would be a connection between two atoms or substructures, be multiple bonds, interconnecting multiple atoms and assign it a score. Does it make, for example, in our case, for a good antibiotic.Eric Topol (07:48):Right. Now, what's also striking as you set up this collaboration that's interdisciplinary with Regina, who I know of her work through breast cancer AI and not through drug discovery and so this was, I think that new effort and this discovery led to this, I love the name of it, Audacious Project, right?Jim Collins (08:13):Right. Yeah, so a few points on the collaboration then I'll speak to Audacious Project. In addition to Regina, we also brought in Tommi Jaakkola, another AI faculty member and marvelous colleague here at MIT and really we've benefited from having outstanding young folks who were multilingual. We had very rich, deep trained grad students from ML on Regina and Tommi's side who appreciated the biology and we had very richly, deeply trained postdocs, Jon Stokes in particular from the microbiology side on my side, who could appreciate the machine learning and so they could speak across the divide. And so, as I look out in the next few decades in this exciting time of AI coming into biomedicine, I think the groups will make a difference of those that have these multilingual young trainees and two who are well set up to also inject human intelligence with machine intelligence.(09:04):Brings the Audacious Project. Now, prior to our publication of halicin, I was invited by the Audacious Project to submit a proposal, the Audacious Project is a new philanthropic effort run by TED, so the group that does the TED Talks that's run by Chris Anderson, so Chris had the idea that there was a need to bring together philanthropists around the world to go for a larger scale in a collective manner toward audacious projects. I pitched them on the idea that we could use AI to address the antibiotic resistance crisis. As you can appreciate, and many of your listeners can appreciate that we're doomed if we don't actually address this soon, in that the number of resistance strains that are in our communities, in our hospitals has been g
“The history of science, it turns out, is filled with stories of very smart people laughing at good ideas.”—Katalin Karikó Ground Truths podcasts are now available on Apple and Spotify!The list of obstacles that Kati Karikó faced to become a scientist, to make any meaningful discovery, to prevail over certain scientists and administrators who oppressed her, unable to obtain grants, her seminal paper rejected by all of the top-tier journals, demoted and dismissed, but ultimately to be awarded the 2023 Nobel Prize with Drew Weissman, is a story for the ages. We covered them in this conversation, which for me will be unforgettable, and hopefully for you an inspiration.Recorded 30 January 2023, unedited transcript belowEric Topol (00:06):Well, hello, this is Eric Topol with Ground Truths, and I am really thrilled to have with me Kati Kariko, who I think everyone knows won the Nobel Prize with the Drew Weissman in 2023 and she has written a sensational book, it's called Breaking Through. I love that title because it's a play on words, a breakthrough and breaking through, and we have a lot to talk about Kati, so welcome.Katalin Kariko (00:34):Thank you very much for inviting me.Eric Topol (00:36):Yes, well I'd like to start off, as you did in the book with your background in Hungary where of course you started with a tough background in a one room house without running water and you never had exposures to scientists and somehow or other you became interested in science and you attributed some of these things like your biology teacher, Mr. Tóth and the book Stress of Life [by Hans Selye] Could you tell us a little bit more what stimulated you in a career of science?Katalin Kariko (01:18):I have to say that every child is interested in understanding the nature around them and so I was surrounded with nature because we had big garden, we had animals around and it was an exciting thing. The children ask questions and if they try to find an answer and teachers or parents might give the answer, but definitely the school, even elementary school was very stimulating. Teachers, chemistry teacher, figure out how we can make crystals and I was so excited to have my own crystals and things like that and in high school the teachers were so engaging and not like they tried to put all of the information into your brain, but they encourage you to think yourself, so that's all contributed. I think that most of the child in the first, I don't know, six, seven years of their life that’s how they can see their parents behaving, their friends, the school, classmates, and they shaped what kind of people they will be at the end and the rest of it is refining.Eric Topol (02:41):Right, right. Well one of the things I loved that you brought up in the book was how much you liked the TV show Columbo. That's one of my favorite TV shows of all time and one more thing, one more thing. Can you talk a little bit about Columbo? Because in some ways you were like the Peter Falk of mRNA in terms of one more thing.Katalin Kariko (03:09):Yes, so I realized that we as researchers, we are not called searchers, we researchers, so we are repeating things. Of course everybody knows who committed the crime in Columbo because this is how it starts and you don't have to figure out, but it seems always that things in a different direction you would lead but all the little clues and some of my colleagues said that they as a physician, they have this tunnel vision. So the patient comes and they can figure out probably from some clues that this is the disease and they get back the lab results and others. Then they realize that one or two things is not fitting, but they always so strongly believe their first instinct. What I taught them to focus on those which will not fit because that will lead to the real perpetrator in case of Columbo.(04:23):And so I like the simplicity. I know that what we are doing this research is very over complicated, but we can break down in very simple question, yes or no and then repeating things and many experiments. When I did one was the experiments really the question and the nine of them was like just controls always. I have to have a control for that, control for that and since I work most of the time with my own hands myself, so I had to make sure that I think through that what will be the experimental outcome and then think about that. Do I have a control for that? So that many times in my brain before I performed the experiment in my brain, I predicted that what will be the outcome, of course you never get the outcome what you expect, but at least you have the control that you can exclude a couple of things and so this is how I function usually in the end of the 20th century, 21st century people did not work like I did alone most of the time.Eric Topol (05:35):No, I see how you described it in the book was just so extraordinary and it really was in keeping with this relentless interrogation and that's what I want to get into is particularly the time when you came to the United States in 1985 and the labs that you worked in predominantly in Philadelphia through that period before leaving Penn to go on to BioNTech. So, you first kind of beached in at Temple University with a monster at least as you portray him in the book. I mean it was nice that he picked you up at the airport, you and your family. How do you say his name? Suhadolnik.Eric Topol (06:31):But not only was the lab kind of infested with cockroaches, but also after working there for a number of years, a few years, you then had gotten an offer to go to Johns Hopkins and when you informed him about that he threatened and did everything he could to ruin your career and get you deported. I mean this was just awful. How did you get through that?Katalin Kariko (06:58):As I mentioned later on, I went back and gave a lecture there and I have to say that I always put positivity in forefront, so I learned a lot from him, and he invited me to America. I was always very grateful, and he was kind, and we did very well, and we did a lot of publication. In one issue of biochemistry, we had three papers and two of them I was the first author, so I worked very hard and so he liked that, and he wanted me to stay there. I just learned that from this Selye book that this is what is given and then what I can do, I cannot change him. I cannot change the situation, how I can get out from it and that's what I focused on, so I am not bitter about him. I liked him and the same for other people. When I get an award, I usually thanks to all of these people who try to make my life miserable. They made me work harder.Eric Topol (08:05):Well, but you were very kind like you said when you went back to Temple many years later to give the lecture because what he did to you, I mean he was so vindictive about you potentially leaving his lab, which he demanded that he be called the boss and he was going to basically, he ruined the Johns Hopkins job. He called them and you were so nice and kind when you went back to give the lecture without saying a negative word about him, so I give you credit, when somebody goes low, you went high, which is nice.Katalin Kariko (08:40):It is important, which I learned from the Selye book, that you don't carry any grudge against anybody because it'll poison you and as Selye also said that when you are very frustrated and very upset, the quickest way you can think about how you can release the stress is revenge. He said, don't do that. It escalate. It hit you back. You have to think about how you can be grateful for the same person you were just ready to take some revenge and that's what you have to practice. Sometimes it is difficult to feel that, but I don't have any bad feeling against my chairman who put my stuff on the hallway.Eric Topol (09:24):Oh yeah, I was going to get to that. So then after a short stint at the Uniformed University of Health Science where you had to drive three hours from Philadelphia to go there and you would sleep on the floor. I mean, I have to say Kati, if I was driving three hours, all I'd be thinking about is how desperate situation I was put in by the prior PI you work with. Any rate, you work there and then finally you got a job with my friend Elliot Barnathan, a cardiologist at University of Pennsylvania. So here you are, you're very interested in mRNA and you hook up with Elliot who's interested in plasminogen activators, and you work in his lab and it's quite a story where one of the students in his lab, David Langer, ratted on you for being blunt about the experiments getting screwed up and then later you wind up working in his lab. Tell me a bit about the times with Elliot because he's a very gracious, I think he was very supportive of your efforts and you got him stimulated about the potential for mRNA, it seems like.Katalin Kariko (10:41):Yes, so I was desperate to be away from my family at Bethesda and try to get back and every day I sent out several applications. This was in 1989, so you had to send letters and then I called up usually the secretaries about what's going on and I called up also a secretary and she said that they were advertised because nobody was good enough. I said, can you ask him to look at again my application? Then half an hour later, Elliot called me back that come and bring your notebook. He wanted to know what kind of experiment I am doing, and he opened when I came a couple of days later and pulled up a northern blot and he said, you have done that? I said, yes, I did. He said, okay, you are hired and so that, because Elliot is just a couple of days younger than me, I convinced him that we should do kind of mRNA research and he agreed, and we did several experiments and he helped me to get all of these experiments ongoing and so it was a very exciting time and I listened. Elliot was there in many awards ceremony including the Nobel Prize. He was my guest because I was very grateful
Jonathan Howard is a neurologist and psychiatrist who practices at NYU-Bellevue and posts frequently on Science Based Medicine.Transcript, unedited, with links to audioEric Topol (00:05):Well, hello, Eric Topol with Ground Truths and I'm really pleased to have the chance to talk with Jonathan Howard today, who is a neurologist and psychiatrist at NYU at Bellevue and has written quite an amazing book published a few months months ago called We Want Them Infected, so welcome Jonathan.Jonathan Howard (00:27):Hey, thanks so much for having me. I really appreciate it.Eric Topol (00:30):Yeah, I mean, there's so much to talk about because we're still in the throes of the pandemic with this current wave at least by wastewater levels and no reason to think it isn't by infections at least the second largest in the pandemic course. I guess I want to start off first with you being into the neuropsychiatric world. How did you become, obviously caring for patients with Covid, but how did you decide to become a Covidologist?Jonathan Howard (00:59):Well, I developed a strong interest in the anti-vaccine movement of all things about a decade ago when a doctor who I trained with here at NYU in Bellevue morphed into one of the country's biggest anti-vaccine doctors a woman by the name of Dr. Kelly Brogan. I knew her well and we were friends; She was smart and after she left NYU in Bellevue, she became one of the country's most outspoken anti-vaccine doctors and really started leaving off the wall things that germ theory didn't exist, that HIV doesn't cause AIDS. When Covid struck, she felt that SARS-CoV-2 was not killing people because she doesn't believe any virus kills people and so I became very fascinated about how smart people can believe strange, incorrect things and I dedicated myself to learning everything that I could about the anti-vaccine movement. In 2018, I wrote a book chapter on the anti-vaccine movement with law professor Dorit Reiss.(02:01):And so when the pandemic came around, I was really prepared for all of their arguments, but I got two very important things wrong. I thought the anti-vaccine movement would shrink. I was wrong about that and I was also really caught off guard by the fact that a lot of mainstream physicians started to parrot pandemic anti-vaccine talking points. So all of the stuff that I'd heard about measles and the HPV vaccine, these are benign viruses, the vaccines weren't tested, blah, blah, blah. I started hearing from professors at Stanford, Harvard, UCSF, Johns Hopkins, all about Covid and the Covid vaccine.Eric Topol (02:40):Yeah, we're going to get to some of the leading institutions and individuals within them and how they were part of this, and surprisingly too, of course. Before we do that in the title of your book, We Want Them Infected, it seems to bring in particularly the Great Barrington Declaration that is just protect the vulnerable elderly and don't worry about the rest. Can you restate that declaration and whether that's a core part of what you were writing about?Jonathan Howard (03:21):Yeah, the title of the book is to be taken literally. It comes from a quote by Dr. Paul Alexander, who was an epidemiologist in the Trump administration and he said in July 4th, 2020, before anyone had been vaccinated, infants, kids, teens, young people, young adults, middle age with no conditions, et cetera, have zero to little risk so we want to use them to develop herd, we want them infected. This was formalized in the Great Barrington Declaration, which was written by three doctors, our epidemiologist, none of whom cared for Covid patients, Jay Bhattacharya at Stanford, Martin Kulldorf who at the time was at Harvard, and Sunetra Gupta who is at Oxford. If I could state their plan in the most generous terms, it would be the following that Covid is much more dangerous for certain people, but we can relatively easily identify older people and people with underlying conditions.(04:19):It's much more benign for a healthy 10-year-old, for example and their idea was that you could separate these two groups, the vulnerable and the not vulnerable. If the not vulnerable people were allowed to catch the virus develop natural immunity that would create herd immunity. They said that this would occur in three to six months and in that time, once herd immunity had been achieved, the vulnerable people who have been in theory sheltering at home are in otherwise safe places could reenter society. So it was really the best of both worlds because lives would be saved and schools would be open, the economy would be open. It sounded very good on paper, kind of like my idea of stopping crime by locking up all the bad guys. What could go wrong? It was a very short document. It took about maybe an hour to write.(05:17):I imagine there were some nefarious forces behind it. One of the main instigators of it was a man by the name of Jeffrey Tucker, who sounds like a cartoon villain and he worked at the, I forget, is the American Enterprise Research Institute. It was some right-wing think tank and he is a literally pro child labor. He wrote an article in 2016 called Let the Kids Work, which suggested that children drop out of school to work at Walmart and Chick-fil-A I'm not making that up and he's overtly pro child smoking. He feels that children, teenagers should smoke because it's cool and then they can quit in their twenties before there are any bad harms from it. Needless to say, the Great Barrington's premises that one infection led to permanent immunity didn't really work out so well, but they were very influential. They had already met with President Trump in August of 2020 and the day after their Great Barrington Declaration was signed, they were invited to the White House. This was October 5th, 2020 to meet with Secretary Human Health and Secretary Services, Alex Azar, and they are advisors to Ron DeSantis. They became mini celebrities over the course of the pandemic and it was a very pro infectious movement. As I said, the title of the book, We Want Them Infected, and they did.Eric Topol (06:42):Right. In fact, I debated Martin Kulldorf, one of the three principals of the Great Barrington Declaration. It was interesting because if you go back to that debate we brought out, at least I tried to highlight the many flaws in this. You've mentioned at least one major flaw, which was to this virus. There's not a long-term immunity built by infections. It's just, as we say with vaccines the immunity for neutralizing antibody production and protection from infections and severe Covid is limited duration for four to six months, and at least for the antibodies and maybe the T-cell immunity is longer, but that doesn't necessarily kick in and quickly. So that was one major flaw, but there are many others, so maybe you could just take that apart further. For example, I like your analogy to lock up all the bad guys, but compartmentalizing people is not so easy in life and I think this is a significant concern of the idea that is, while you indicated there may be some merits if things went as planned, but what else was a flaw of that argument or proposition?Jonathan Howard (08:11):So yeah, this could be a 10-hour conversation and I think importantly, we don't have to speak hypothetically here. A lot of defenders of the Great Barrington Declaration will say, oh, we never tried it, but they promised that herd immunity would arrive in three to six months after lockdowns ended. So we don't have to speak theoretically about what would've happened had we done it. Lockdowns ended a while ago and we don't have herd immunity. They were very clear on this. Dr. Kulldorf tweeted in December 2020 that if we use focus protection, the pandemic will be over in three to six months. So, what could have gone wrong if about 250 million unvaccinated Americans contracted Covid simultaneously in October and November of 2020? A lot of things, as we said, they dichotomized people into vulnerable and not vulnerable, but of course it exists on this. The only bad outcome they recognized was death.(09:11):They felt that either you died or you had the sniffle for a few days and you emerged unscathed. Separating vulnerable people from not vulnerable people is a lot easier than it sounds and I think by way of comparison, look at the mRNA vaccine trials. You can read their protocols and the protocols for these trials were 300-400 pages of dense policies and procedures. The Great Barrington Declaration, if you go to their frequently asked questions section, they made some suggestions, which sound great, like older people should have food delivered at home during times of high transmission, but setting up a national or even statewide food delivery program, that's a lot harder than it sounds. When asked about that later, Dr. Bhattacharya has said they could have used DoorDash, for example. So it was just very clear that no serious thought went into this because it was really an unactionable thing.(10:21):It's not as if public health officials had billions of dollars at their disposal and they weren't many dictators. They couldn't set up home food delivery programs overnight like they suggested and two months after the Great Barrington Declaration was published, vaccines became available so it became obsolete. Not that vaccines have turned out to be the perfect panacea that we had hoped for, unfortunately, but the idea that young people should continue to try to get natural low immunity in favor instead of vaccination became at that point obscene, but they still are anti-vaccine for young people and for children, which I find despicable at this point.Eric Topol (11:07):Right, the data is unequivocal that there's benefit across the board. In fact, just last week in JAMA two senior people at FDA, Peter Marks and Robert Califf published the graphs of how across all ages there was reduction in mortality with the vaccines. That gets us to, as you say now into
is an award-wining entrepreneur and innovator in technology, especially A.I., a member of the editorial board of Harvard Business Review, and an outstanding communicator which makes him a frequent media guest and often featured in The Economist, WSJ, and Financial Times. is chock full of interesting analyses and podcasts on tech and A.I. Here’s his summary of our extended and fun discussionI hope you find our conversation interesting and informative. Get full access to Ground Truths at erictopol.substack.com/subscribe
A snippet of our conversation belowTranscript of our conversation 8 January 2023, edited for accuracy, with external linksEric TopolIt’s a pleasure for me to have Liv Boeree as our Ground Truths podcast guest today. I met her at the TED meeting in October dedicated to AI. I think she's one of the most interesting people I’ve met in years and the first time I've ever interviewed a professional poker player who has won world championships and we're going to go through that whole story, so welcome Liv.Liv BoereeThanks for having me, Eric.Eric TopolYou have an amazing background having been at the University of Manchester in physics and astrophysics. Back around in 2005 you landed into the poker world. Maybe you could help us understand how you went from physics to poker.From Physics to PokerLiv BoereeAh, yeah. It's a strange story, I graduated as you said in 2005 and I had student debt and needed to get a job I had plans to continue in academia. I wanted to do a masters and then a PhD to work in astrophysics in some way, but I needed to make some money, so I started applying for TV game shows and it was on one of these game shows that I first learned how to play poker. They were looking for beginners and the loose premise of the show was which personality type is best suited for learning the game and even though I didn't win that particular show we were playing for a winner take all prize of £100,000 which was a life changing amount of money had I won it at the time. It was like a light bulb moment just the game and I’ve always been a very competitive person, but poker in particular really spoke to my soul. I always wanted to play in games where it was often considered a boy’s game and I could be a girl beating the boys at their own game. I hadn't played that much cards in particular, but I just loved any game that was very cutthroat which poker certainly is. From that point onwards I was like you know what I'm going to put physics on hold and see if I can make it in this poker world instead and then never really looked back.Eric TopolWell, you sure made it in that world. I know you retired back in about 2019, but that was after you won all sorts of world and European championships and beat a lot of men. No less. What were some of the things that that made you such a phenomenal player?Liv BoereeThe main thing with poker is well the most important ingredient if you really want to make it as a professional is you have to be extremely competitive. I have not met any top pros who don't have that degree of killer instinct when it comes to the game that doesn't mean it means you're competitive in everything else in life, but you have to have a passion for looking someone in the eye, mentally modeling them, thinking how to outwit them and put them into difficult situations within the game and then take pleasure in that. So, there’s a certain personality type that tends to enjoy that. The other key facet is you have to be comfortable with thinking in terms of probability. The cards are shuffled between every hand so there's this inherent degree of randomness. On the scale of pure roulette which is all luck no skill to a game like chess which has almost no luck (close to 100% skill as you can get) poker lies somewhere in the middle and of course the more you play the bigger the skill edge and the smaller the luck factor. That's why professionals can exist. It's a game of both luck and skill which I think is what makes it so interesting because that's what life is really, right? We're trying to get our business off the ground, we're trying to compete in the dating market. Whatever it is. We're doing our strategy, the role of luck life can throw your curved balls that you can do everything right and still things don't go the way you intended them to or vice versa, but there's also strategies we can employ to improve our chances of success. Those are the sort of skills that poker players particularly this idea of gray scale probabilistic thinking that you really have to hone. I've always wondered whether having a background in science or at least you know studying having ah a scientific degree helped in that regard because of course the scientific method is about understanding variables and minimizing uncertainty as much as possible and understanding what cofounding factors can bias the outcome of your results. Again, that's always going on in a poker player's mind, you'll have concurrent hypotheses. Oh, this guy just made a huge bet into me when that ace came out, is it because he actually has an ace or is it because he's pretending to have an ace and so you've got to weigh all the bits of information up as unbiased as possible in an unbiased way as possible to come to a correct conclusion. Even then you can never be certain, so this idea of understanding biases understanding probabilities I think that’s why a lot of top poker players have backgrounds in scientific degrees a very good friend of mine he had a PhD in in physics. Especially over time poker has become a much more sort of scientific pursuit. When I first allowed to play it was very much a game of street smarts and intuition in part because we didn't have the technological tools to understand really the mechanics of the game as well. You couldn't record all your playing data if you were playing just in a casino unless you were writing down your hands. Otherwise, this information wasn't getting stored anywhere, but then online poker came along which meant that you could store all this data on your laptop and then build tools to analyze that data and so the game became a much more technical scientific pursuit.Eric TopolThat actually gets to kind of the human side of poker. Not the online version —especially since we're going to be mainly talking about AI the term “poker face” the ability to bluff is that a big part of this?Liv BoereeOh, absolutely. You can't be a good poker player if you don't ever bluff because your opponents will start to notice that so that means you're only ever putting your money on the line when you have a good hand so why would they ever pay you off. The point of poker is to maximize the deception to your opponents so you have to use strategies where some of the time you might be having a strong hand and some of the time you might be bluffing where you might have a weak hand. The key is this is getting into the technical sort of game theory side of it, but you want to be doing these bluffs versus what we call value bets as in betting with a good hand with the right to sort of frequency. You need these right ratios between them, so bluffing is a very core part of the game and yes having a poker face obviously helps because you want to be as inscrutable to your opponents as possible. At the same time online poker is an enormously popular game where you can't see your opponent's faces.Eric TopolRight, right.Liv BoereeYet you can still bluff which could actually lead us into this topic of AI because now the best players in the world are actually AIs.Eric TopolWell, it's interesting because it takes out that human component of being able to bluff and it may be good for people who don't have a poker face. They can play online poker and be good at it because they don't have that disguise if you will.Liv BoereeRight.Game Theory and Moloch TrapsEric TopolThat gets me to game theory and a big part of the talk you gave at the TED conference about something that I think a lot of the folks listening aren't familiar with— Moloch traps. Could you enlighten us about that because what the talk which of course we’ll link to is so illuminating and apropos to the AI landscape that we face today?Liv BoereeYeah, I’ll leave it for people to go and watch the TED talk because that's going to be much more succinct than me to explain the backstory of how it came to be called a Moloch trap because Moloch is a sort of biblical figure a demon and it seems strange that you would be applying such a concept to what's basically a collection of game theoretic incentives, but essentially what a Moloch trap is the more formal name for it is a multipolar trap which some of the listeners may be familiar with. Essentially a Moloch trap or a multipolar trap is one of those situations where you have a lot of competing different people all competing for 1 particular thing that say who can collect the most fish out of a lake. The trap occurs when everyone is incentivized to get as much of that thing as possible so to go for a specific objective, but if everyone ends up doing it then the overall environment ends up being worse off than before. What we're seeing with plastic pollution – It’s not like packaging companies want to fill the oceans with plastic. They don't want this outcome. It doesn't make them look good. They're all caught on the trap of needing to maximize profits and external and one of the most efficient ways of doing that is to externalize costs outside of their P&L by using cheap packaging that perhaps ends up in the lakes or the oceans and if everyone ends up doing this but well basically you're a CEO in a decision of I could do the more expensive selfless action, but if I don't do that then I know that my competitors are going to do the selfish thing. I might as well do it anyway because the world's going to end up in roughly the same outcome whether I do it or not because everyone ends up adopting this mindset they end up being trapped in this bad situation. Another way of thinking of it is if you're watching a football at a stadium or a concert and before the show starts everyone's sitting down, but then a few people near the front want to get a better view so they stand up. That now forces the people right behind them to make a decision. I don't really want to block the people behind me but I can't see anymore, so now I have to stand up. The whole thing sort of falls down until everyone is now stuck standing for the rest of the show. No one really actually has a
The science to advance our understanding of the aging process—and to potentially slow it down—has made important strides. One of the leading scientists responsible for this work is Professor Tony Wyss-Coray, whose work has particularly focused on brain aging but has implications for all organs. I believe his December 2023 Nature paper on blood proteins that can track aging for 11 of our organs is one of the most important aging reports yet.Here is the audio and transcript of our conversation, recorded 20 December 2023, with a few relevant external links.This is the last Ground Truths post for 2023 and I hope you’ll find it informative. I look forward to sharing many more exciting, cutting-edge biomedical advances with you in 2024!00:10.38Eric TopolHello this is Eric Topol and for this edition of Ground Truths. I'm so delighted to have with me Professor Tony Wyss-Coray of Stanford, a Distinguished Professor at Stanford and who directs the Knight Initiative for Brain Resilience. So welcome Tony.00:30.19Tony Wyss-CorayThank you, thank you for having me, Eric.00:32.84Eric TopolWell, I've been following your career and your work for decades I have to say and what you just published a couple weeks ago in Nature. The cover paper about internal organ clocks. It blew me away. I mean it's a built on a foundation of extraordinary work. I thought we could start with that because to me that's really a breakthrough in that when we think of aging and how to gauge a person aging with things like the Horvath clock of methylation markers or telomeres or —not at all specific to any part of the body, just overall, l but you published an extraordinary work about plasma proteins for 11 organs that predicted the outcomes things like heart failure and Alzheimer's so maybe you could tell us about this. Seems to be a big deal to me.01:28.41Tony Wyss-CorayThank you so much I'm honored. Really, you know I think if you work on this stuff, especially for several years it feels sort of obvious to do it? But I think you know it is in a way. It is. Pretty simple. So what we argued is that the thousands of proteins that you know are present in our blood. They must originate from somewhere now a lot of proteins are you know, produced by cells throughout the body. But some proteins are very specifically produced. For example, only in the brain or only in the liver or only in the heart because they have specialized functions and we have you know being taking advantage of that in clinical medicine where you measure. Often you know one of these proteins to sort of diagnose pathology in a tissue, but we took this It's just a level further and said, well, let's just find out of thousands of proteins that we can measure assign them to specific organs and tissues. And then see whether they change with age and many of them turn out to change. We found you know about 1500 proteins or so in the study that we did although that number can grow dramatically if we you know keep.03:01.11Tony Wyss-CorayImproving our technologies or techniques to measure them and many of them come from the brain or from other tissues and because they change with age. They tell us something about the aging of that organ. And as others have shown in the field including Steve Horvath is that that prediction of the age if it doesn't really match exactly your actual age contains information about the state the physiological state or the risk to develop. Organ-specific disease.03:37.75Eric TopolRight. And you found that about 1 in 5 people had evidence of accelerated aging of 1 organ which of course is really starting to nail down ability to detect aging you know to localize it and um. What strikes me Tony is that now because we're seeing at the cusp of advancing in the science of aging a field that you have done so much to propel forward and one of the issues has been well, how are we going to prove it. We can't wait for 20 years to show that. Whatever intervention led to promotion of healthy aging. But when you have a marker like this of organ specificity, it seems like the chances of being able to show that intervention makes a difference is enhanced would you say so?04:29.28Tony Wyss-CorayYeah, absolutely I think that's one of the most exciting aspects of this that we can now start looking at interventions whether they are you know a specific intervention that tries to target the aging process, or you know just that. Let's say a cholesterol lowering drug or blood pressure lowering drug does that have a beneficial effect on the heart. For example, on the kidney or you can also start thinking of lifestyle interventions where they actually have an effect right? If you started exercising you collect your blood before and then a year after you have an exercise regimen does that actually change the age that we can measure with these different clocks.05:22.55Eric TopolRight? Well I mean it's really a striking advance and by a marker of aging so that gets me to your other work. You've done well over 10 years which is that you could identify that given young blood. First of course in mice and then later verified in people could improve cognitive function in older whether it's experimental models or in people. So what are your thoughts about that is that if that's something you've been ruminating on for many years and I’m sure there are places around the world that are trying to do this sort of thing. What do you think of that potential?06:11.40Tony Wyss-CorayYeah, so there really this recent observation or study really came out of you know that finding that young blood can change the age of different organs and you know we. We were not the first to show this. We showed it for the brain but Tom Rando who studied muscle stem cell aging showed this you know a few years earlier in the muscle and we worked with Tom to explore this for the brain, but it shows sort of that this you know the composition of the blood. It is really not just reflecting the age of organs and tissues. But it actually also affects them. It directs them in a way and so you can speculate that you know if you had an organ that shows accelerated aging. Because some of the factors end up in the blood. They might actually induce aging in other tissues and so promote the aging process and people in the field have also shown that this is true for specific cells. We call them senescence cells. So these are a specific type of cell that seem to somehow stop dividing and assume the state that releases inflammatory factors these cells too. They seem to almost infect the neighborhood where they live in with an age promoting sort of.07:41.95Tony Wyss-CorayThe secretome , as we call it, so they release factors that seem to promote aging locally but potentially across the organism and interfering in that could potentially have rejuvenating effects and so that brings us back to this observation that.08:01.23Tony Wyss-CorayYoung blood could potentially rejuvenate organs We know old blood can accelerate it at least in mice. So could we neutralize the age promoting factors in people and could we deliver sort of the rejuvenating factors. Now what's been frustrating for me is that it has been incredibly challenging to identify the key factors.08:33.30Tony Wyss-CorayI think we became to realize as a field that there is not 1 factor. There's not 1 magic factor that will keep us young or keep our organs young but rather different cells and different organs in our body seem to respond in different ways actually to this young blood. Can show this with molecular tools. We can show that every cell actually responds. So if you take a mouse an old mouse and you give it young blood every cell in that mouse shows a transcription of the response to the young blood.09:10.80Tony Wyss-CoraySome of them may regenerate mitochondria and others activate other pathways. We see that stem cells respond particularly well the stem cells of the Immune system hematopoietic stem cells um while other cells show less of a response. And that to me suggests that they respond to different factors in the young blood and that you know they have very specific um receptors Probably that recognize some of these beneficial factors and then respond in a specific way. So that’s what we need to.09:33.16Eric TopolRight.09:48.63Tony Wyss-CorayFigure out I think as a field to translate this really to the clinic is what are the key factors and will it be possible to make a cocktail that sort of mimics Nature's you know elixir10:06.13Tony Wyss-CorayI Said this before it's almost like the fountain of youth is within us, but it just dries out as we get older and if we could figure out what are the key factors that that make up this fountain. We could potentially you know either, as a treatment, deliver it again or reactivate that found and so that the body produces these factors again.10:34.73Eric TopolWell, you know that's something that years ago I was very skeptical about and because of your work and others in the field. I've come a long way thinking that we're on the cusp of really identifying ways to truly promote healthy aging. And so this is a really you know extraordinary time in our lives I wonder you of course mentioned 2 critical paths that have been identified the senescent cells—removing them— or the infusion of young plasma. Would you say it's too simplistic to reduce this to decreasing inflammation or is that really the theme here, or is it much more involved than that.11:28.48Tony Wyss-CorayI think inflammation has a big part in that but you know inflammation is such a broad term and such an ill-defined term that um yeah I can say yes to your question.11:44.45Tony Wyss-CorayAnd I'm probably not going to be wrong. Um, but if we really want to know which molecular pathways in the inflammatory cascade are key to this detrimental process that seems to accelerate aging. Um, I think we have to work a bit harder and really so define what we're saying you can't just have thousan
David Liu is an gifted molecular biologist and chemist who has pioneered major refinements in how we are and will be doing genome editing in the future, validating the methods in multiple experimental models, and establishing multiple companies to accelerate their progress.The interview that follows here highlights why those refinements beyond the CRISPR Cas9 nuclease (used for sickle cell disease) are vital, how we can achieve better delivery of editing packages into cells, ethical dilemmas, and a future of somatic (body) cell genome editing that is in some ways is up to our imagination, because of its breadth, over the many years ahead. Recorded 29 November 2023 (knowing the FDA approval for sickle cell disease was imminent)Annotated with figures, external links to promote understanding, highlights in bold or italics, along with audio links (underlined)Eric Topol (00:11):Hello, this is Eric Topol with Ground Truths and I'm so thrilled to have David Liu with me today from the Broad Institute, Harvard, and an HHMI Investigator. David was here visiting at Scripps Research in the spring, gave an incredible talk which I'll put a link to. We're not going to try to go over all that stuff today, but what a time to be able to get to talk with you about what's happening, David. So welcome.David Liu (00:36):Thank you, and I'm honored to be here.Eric Topol (00:39):Well, the recent UK approval (November 16, 2023) of the first genome editing after all the years that you put into this, along with many other colleagues around the world, is pretty extraordinary. Maybe you can just give us a sense of that threshold that's crossed with the sickle cell and beta thalassemia also imminently [FDA approval granted for sickle-cell on 8 December 2023] likely to be getting that same approval here in the U.S.David Liu (01:05):Right? I mean, it is a huge moment for the field, for science, for medicine. And just to be clear and to give credit where credit is due, I had nothing to do with the discovery or development of CRISPR Cas9 as a therapeutic, which is what this initial gene editing CRISPR drug is. But of course, the field has built on the work of many scientists with respect to CRISPR Cas9, including Emmanuel Charpentier and Jennifer Doudna and George Church and Feng Zhang and many, many others. But it is, I think surprisingly rapid milestone in a long decade’s old effort to begin to take some control over our genetic features by changing DNA sequences of our choosing into sequences that we believe will offer some therapeutic benefit. So this initial drug is the CRISPR Therapeutics /Vertex drug. Now we can say it's actually a drug approved drug, which is a Crispr Cas9 nuclease programmed to cut a DNA sequence that is involved in silencing fetal hemoglobin genes. And as you know, when you cut DNA, you primarily disrupt the sequence that you cut. And so if you disrupt the DNA sequence that is required for silencing your backup fetal hemoglobin genes, then they can reawaken and serve as a way to compensate for adult hemoglobin genes like the defective sickle cell alleles that sickle cell anemia patients have. And so that's the scientific basis of this initial drug.Eric Topol (03:12):So as you aptly put— frame this—this is an outgrowth of about a decade's work and it was using a somewhat constrained, rudimentary form of editing. And your work has taken this field considerably further with base and prime editing whereby you're not just making a double strand cut, you're doing nicks, and maybe you can help us understand this next phase where you have more ways you can intervene in the genome than was possible through the original Cas9 nucleases.David Liu (03:53):Right? So gene editing is actually a several decades old field. It just didn't quite become as popular as it is now until the discovery of CRISPR nucleases, which are just much easier to reprogram than the previous programmable zinc finger or tail nucleases, for example. So the first class of gene editing agents are all nuclease enzymes, meaning enzymes that take a piece of DNA chromosome and literally cut it breaking the DNA double helix and cutting the chromosome into two pieces. So when the cell sees that double strand DNA break, it responds by trying to get the broken ends of the chromosome back together. And we think that most of the time, maybe 90% of the time that end joining is perfect, it just regenerates the starting sequence. But if it regenerates the starting sequence perfectly and the nuclease is still around, then it can just cut the rejoin sequence again.(04:56):So this cycle of cutting and rejoining and cutting and rejoining continues over and over until the rejoining makes the mistake that changes the DNA sequence at the cut site because when those mistakes accumulate to a point that the nuclease no longer recognizes the altered sequence, then it's a dead end product. That's how you end up with these disrupted genes that result from cutting a target DNA sequence with a nuclease like Crispr Cas9. So Crispr Cas9 and other nucleases are very useful for disrupting genes, but one of their biggest downsides is in the cells that are most relevant to medicine, to human therapy like the cells that are in your body right now, you can't really control the sequence of DNA that comes out of this process when you cut a DNA double helix inside of a human cell and allow this cutting and rejoining process to take place over and over again until you get these mistakes.(06:03):Those mistakes are generally mixtures of insertions and deletions that we can't control. They are usually disruptive to a gene. So that can be very useful when you're trying to disrupt the function of a gene like the genes that are involved in silencing fetal hemoglobin. But if you want to precisely fix a mutation that causes a genetic disease and convert it, for example, back into a healthy DNA sequence, that's very hard to do in a patient using DNA cutting scissors because the scissors themselves of course don't include any information that allows you to control what sequence comes out of that repair process. You can add a DNA template to this cutting process in a process called HDR or Homology Directed Repair (figure below from the Wang and Doudna 10-year Science review), and sometimes that template will end up replacing the DNA sequence around the cut site. But unfortunately, we now know that that HDR process is very inefficient in most of the types of cells that are relevant for human therapy.(07:12):And that explains why if you look at the 50 plus nuclease gene editing clinical trials that are underway or have taken place, all but one use nucleases for gene disruption rather than for gene correction. And so that's really what inspired us to develop base editing in 2016 and then prime editing in 2019. These are methods that allow you to change a DNA sequence of your choosing into a different sequence of your choosing, where you get to specify the sequence that comes out of the editing process. And that means you can, for the first time in a general way, programmable change a DNA sequence, a mutation that causes a genetic disease, for example, into a healthy sequence back into the normal, the so-called wild type sequence, for example. So base editors work by actually performing chemistry on an individual DNA base, rearranging the atoms of that base to become a different base.(08:22):So base editors can efficiently and robustly change A's into G's G's, into A's T's into C's or C's into T's. Those four changes. And those four changes for interesting biochemical reasons turn out to be four of the most common ways that our DNA mutates to cause disease. So base editors can be used and have been used in animals and now in six clinical trials to treat a wide variety of diseases, high cholesterol and sickle cell disease, and T-cell leukemia for example. And then in prime editors we developed a few years later to try to address the types of changes in our genomes that caused genetic disease that can't be fixed with a base editor, for example. You can't use a base editor to efficiently and selectively change an A into a T. You can't use a base editor to perform an insertion of missing DNA letters like the three missing letters, CTT, that's the most common cause of cystic fibrosis accounting for maybe 70% of cystic fibrosis patients.(09:42):You can't use a base editor to insert missing DNA letters like the missing TATC. That is the most common cause of Tay-Sachs disease. So we develop prime editors as a third gene editing technology to complement nucleases and base editors. And prime editors work by yet another mechanism. They don't, again, they don't cut the DNA double helix, at least they don't cause that as the required mechanism of editing. They don't perform chemistry on an individual base. Instead, prime editors take a target DNA sequence and then write a new DNA sequence onto the end of one of the DNA strands and then sort of help the cell navigate the DNA repair processes to have that newly written DNA sequence replace the original DNA sequence. And in the process it's sort of true search and replace gene editing. So you can basically take any DNA sequence of up to now hundreds of base pairs and replace it with any other sequence of your choosing of up to hundreds of base pairs. And if you integrate prime editing with other enzymes like recombinase, you can actually perform whole gene integration of five or 10,000 base pairs, for example, this way. So prime editing's hallmark is really its versatility. And even though it's the newest of the three ways that have been robustly used to edit mammalian cells and rescue animal models of genetic disease, it is arguably the most versatile by far,Eric Topol (11:24):Right? Well, in fact, if you just go back to the sickle cell story as you laid out the Cas9 nuclease, that's now going into commercial approval in the UK and the US, it's more of a blunt instrument of dis
This is one of the most enthralling and fun interviews I’ve ever done (in 2 decades of doing them) and I hope that you’ll find it stimulating and provocative. If you did, please share with your network.And thanks for listening, reading, and subscribing to Ground Truths.Recorded 4 December 2023Transcript below with external links to relevant material along with links to the audioERIC TOPOL (00:00):This is for me a real delight to have the chance to have a conversation with Geoffrey Hinton. I followed his work for years, but this is the first time we've actually had a chance to meet. And so this is for me, one of the real highlights of our Ground Truths podcast. So welcome Geoff.GEOFFREY HINTON (00:21):Thank you very much. It's a real opportunity for me too. You're an expert in one area. I'm an expert in another and it's great to meet up.ERIC TOPOL (00:29):Well, this is a real point of conversion if there ever was one. And I guess maybe I'd start off with, you've been in the news a lot lately, of course, but what piqued my interest to connect with you was your interview on 60 Minutes with Scott Pelley. You said: “An obvious area where there's huge benefits is healthcare. AI is already comparable with radiologists understanding what's going on in medical images. It's going to be very good at designing drugs. It already is designing drugs. So that's an area where it's almost entirely going to do good. I like that area.”I love that quote Geoff, and I thought maybe we could start with that.GEOFFREY HINTON (01:14):Yeah. Back in 2012, one of my graduate students called George Dahl who did speech recognition in 2009, made a big difference there. Entered a competition by Merck Frost to predict how well particular chemicals would bind to something. He knew nothing about the science of it. All he had was a few thousand descriptors of each of these chemicals and 15 targets that things might bind to. And he used the same network as we used for speech recognition. So he treated the 2000 descriptors of chemicals as if they were things in a spectrogram for speech. And he won the competition. And after he'd won the competition, he wasn't allowed to collect the $20,000 prize until he told Merck how he did it. And one of their questions was, what qsar did you use? So, he said, what's qsar? Now qsar is a field, it has a journal, it's had a conference, it's been going for many years, and it's the field of quantitative structural activity relationships. And that's the field that tries to predict whether some chemical is going to bind to something. And basically he'd wiped out that field without knowing its name.ERIC TOPOL (02:46):Well, it's striking how healthcare, medicine, life science has had somewhat of a separate path in recent AI with transformer models and also going back of course to the phenomenal work you did with the era of bringing in deep learning and deep neural networks. But I guess what I thought I'd start with here with that healthcare may have a special edge versus its use in other areas because, of course, there's concerns which you and others have raised regarding safety, the potential, not just hallucinations and confabulation of course a better term or the negative consequences of where AI is headed. But would you say that the medical life science AlphaFold2 is another example of from your colleagues Demis Hassabis and others at Google DeepMind where this is something that has a much more optimistic look?GEOFFREY HINTON (04:00):Absolutely. I mean, I always pivot to medicine as an example of all the good it can do because almost everything it's going to do there is going to be good. There are some bad uses like trying to figure out who to not insure, but they're relatively limited almost certainly it's going to be extremely helpful. We're going to have a family doctor who's seen a hundred million patients and they're going to be a much better family doctor.ERIC TOPOL (04:27):Well, that's really an important note. And that gets us to a paper preprint that was just published yesterday, on arXiv, which interestingly isn't usually the one that publishes a lot of medical preprints, but it was done by folks at Google who later informed me was a model large language model that hadn't yet been publicized. They wouldn't disclose the name and it wasn't MedPaLM2. But nonetheless, it was a very unique study because it randomized their LLM in 20 internists with about nine years of experience in medical practice for answering over 300 clinical pathologic conferences of the New England Journal. These are the case reports where the master clinician is brought in to try to come up with a differential diagnosis. And the striking thing on that report, which is perhaps the best yet about medical diagnoses, and it gets back Geoff to your hundred million visits, is that the LLM exceeded the clinicians in this randomized study for coming up with a differential diagnosis. I wonder what your thoughts are on this.GEOFFREY HINTON (05:59):So in 2016, I made a daring and incorrect prediction was that within five years, the neural nets were going to be better than radiologists that interpreting medical scans, it was sometimes taken out of context. I meant it for interpreting medical scans, not for doing everything a radiologist does, and I was wrong about that. But at the present time, they're comparable. This is like seven years later. They're comparable with radiologists for many different kinds of medical scans. And I believe that in 10 years they'll be routinely used to give a second opinion and maybe in 15 years they'll be so good at giving second opinions that the doctor's opinion will be the second one. And so I think I was off by about a factor of three, but I'm still convinced I was completely right in the long term.(06:55):So this paper that you're referring to, there are actually two people from the Toronto Google Lab as authors of that paper. And like you say, it was based on the large language PaLM2 model that was then fine-tuned. It was fine-tuned slightly differently from MedPaLM2 I believe, but the LLM [large language model] by themselves seemed to be better than the internists. But what was more interesting was the LLMs when used by the internists made the internists much better. If I remember right, they were like 15% better when they used the LLMs and only 8% better when they used Google search and the medical literature. So certainly the case that as a second opinion, they're really already extremely useful.ERIC TOPOL (07:48):It gets again, to your point about that corpus of knowledge that is incorporated in the LLM is providing a differential diagnosis that might not come to the mind of the physician. And this is of course the edge of having ingested so much and being able to play back those possibilities and the differential diagnosis. If it isn't in your list, it's certainly not going to be your final diagnosis. I do want to get back to the radiologist because we're talking just after the annual massive Chicago Radiologic Society of North America RSNA meeting. And at those meetings, I wasn't there, but talking to my radiology colleagues, they say that your projection is already happening. Now that is the ability to not just read, make the report. I mean the whole works. So it may not have been five years when you said that, which is one of the most frequent quotes in all of AI and medicine of course, as you probably know, but it's approximating your prognosis. Even nowGEOFFREY HINTON (09:02):I've learned one thing about medicine, which is just like other academics, doctors have egos and saying this stuff is going to replace them is not the right move. The right move is to say it's going to be very good at giving second opinions, but the doctor's still going to be in charge. And that's clearly the way to sell things. And that's fine, just I actually believe that after a while of that, you'll be listening to the AI system, not the doctors. And of course there's dangers in that. So we've seen the dangers in face recognition where if you train on a database that contains very few black people, you'll get something that's very good at recognizing faces. And the people who use it, the police will think this is good at recognizing faces. And when it gives you the wrong identity for a person of color, then the policemen are going to believe it. And that's a disaster. And we might get the same with medicine. If there's some small minority group that has some distinctly different probabilities of different diseases, it's quite dangerous for doctors to get to trust these things if they haven't been very carefully controlled for the training data.ERIC TOPOL (10:17):Right. And actually I did want to get back to you. Is it possible for the reason why in this new report that the LLMs did so well is that some of these case studies from New England Journal were part of the pre-training?GEOFFREY HINTON (10:32):That is always a big worry. It's worried me a lot and it's worried other people a lot because these things have pulled in so much data. There is now a way round that at least for showing that the LLMs are genuinely creative. So he's a very good computer science theorist at Princeton called Sanjeev Arora, and I'm going to attribute all this to him, but of course, all the work was done by his students and postdocs and collaborators. And the idea is you can get these language models to generate stuff, but you can then put constraints on what they generate by saying, so I tried an example recently, I took two Toronto newspapers and said, compare these two newspapers using three or four sentences, and in your answer demonstrate sarcasm, a red herring empathy, and there's something else. But I forget what metaphor. Metaphor.ERIC TOPOL (11:29):Oh yeah.GEOFFREY HINTON (11:29):And it gave a brilliant comparison of the two newspapers exhibiting all those things. And the point of Sanjeev Arora’s work is that if you have a large number of t
“A.I. is not the problem; it’s the solution.”—Andrew Ng at TED, 17 October 2023Recorded 21 November 2023Transcript with relevant links and links to audio fileEric Topol (00:00):Hello, it's Eric Topol with Ground Truths, and I'm really delighted to have with me Andrew Ng, who is a giant in AI who I've gotten to know over the years and have the highest regard. So Andrew, welcome.Andrew Ng (00:14): Hey, thanks Eric. It's always a pleasure to see you.Eric Topol (00:16):Yeah, we've had some intersections in multiple areas of AI. The one I wanted to start with is that you've had some direct healthcare nurturing and we've had the pleasure of working with Woebot Health, particularly with Alison Darcy, where the AI chatbot has been tested in randomized trials to help people with depression and anxiety. And, of course, that was a chatbot in the pre-transformer or pre-LLM era. I wonder if you could just comment about that as well as your outlook for current AI models in healthcare.Andrew Ng (01:05):So Alyson Darcy is brilliant. It's been such a privilege to work with her over the years. One of the exciting things about AI is a general purpose technology. It's not useful for one thing. And I think in healthcare and more broadly across the world, we're seeing many creative people use AI for many different applications. So I was in Singapore a couple months ago and I was chatting with some folks, Dean Chang and one of his doctors, Dr. M, about how they're using AI to read EHRs in a hospital in Singapore to try to estimate how long a patient's going to be in the hospital because of pneumonia or something. And it was actually triggering helpful for conversations where a doctor say, oh, I think this patient will be in for three days, but the AI says no, I'm guessing 15 days. And this triggers a conversation where the doctor takes a more careful look. And I thought that was incredible. So all around the world, many innovators everywhere, finding very creative ways to apply AI to lots of different problems. I think that's super exciting.Eric Topol (02:06):Oh, it's extraordinary to me. I think Geoff Hinton has thought that the most important application of current AI is in the healthcare/ medical sphere. But I think that the range here is quite extraordinary. And one of the other things that you've been into for all these years with Coursera starting that and all the courses for deep learning.AI —the democratization of knowledge and education in AI. Since this is something like all patients would want to look up on whatever GPT-X about their symptoms different than of course a current Google search. What's your sense about the ability to use generative AI in this way?Andrew Ng (02:59):I think that instead of seeing a doctor as a large language model, what's up with my symptoms, people are definitely doing it. And there have been anecdotes of this maybe saving a few people's lives even. And I think in the United States we're privileged to have some would say terrible, but certainly better than many other country’s healthcare system. And I feel like a lot of the early go-to market for AI enabled healthcare may end up being in countries or just places with less access to doctors. The definitely countries where you can either decide do you want to go see if someone falls sick? You can either send your kid to a doctor or you can have your family eat for the next two weeks, pick one. So with families made these impossible decisions, I wish we could give everyone in the world access to a great doctor and sometimes the alternatives that people face are pretty harsh. I think any hope, even the very imperfect hope of LLM, I know it sounds terrible, it will hallucinate, it will give bad medical advice sometimes, but is that better than no medical advice? I think there's really some tough ethical questions are being debated around the world right now.Eric Topol (04:18):Those hallucinations or confabulation, won't they get better over time?Andrew Ng (04:24):Yes, I think LLM technology is advanced rapidly. They still do hallucinate, they do still mix stuff up, but it turns out that I think people still have an impression of LLM technology from six months ago. But so much has changed in the last six months. So even in the last six months, it is actually much harder now to get an LMM, at least many of the public ones offered by launch companies. It's much harder now compared to six months ago to get it to give you deliberately harmful advice or if you ask it for detailed instructions on how to commit a crime. Six months ago it was actually pretty easy. So that was not good. But now it's actually pretty hard. It's not impossible. And I actually ask LLMs for strange things all the time just to test them. And yes, sometimes I can get them when I really try to do something inappropriate, but it's actually pretty difficult.(05:13):But hallucination is just a different thing where LLMs do mix stuff up and you definitely don't want that when it comes to medical advice. So it'll be an interesting balance I think of when should we use web search for trust authoritative sources. So if I have a sprained ankle, hey, let me just find a webpage on trust from a trusted medical authority on how to deal with sprained ankle. But there are also a lot of things where there is no one webpage that just gives me an answer. And then this is an alternative for generating a novel thing that's need to my situation. In non-healthcare cases, this has clearly been very valuable in just the healthcare, given the criticality of human health and human life. I think people are wrestling with some challenging questions, but hallucinations are slowly going down.Eric Topol (05:59):Well, hopefully they'll continue to improve on that. And as you pointed out the other guardrails that will help. Now that gets me to a little over a month ago, we were at the TED AI program and you gave the opening talk, which was very inspirational, and you basically challenged the critics of the negativism on AI with three basic issues: amplifying our worst impulses, taking our jobs and wiping out humanity. And it was very compelling and I hope that that will be posted soon. And of course we'll link it, but can you give us a skinny of your antidote to the doomerism about AI?Andrew Ng (06:46):Yeah, so I think AI is a very beneficial technology on average. I think it comes down to do we think the world is better off or worse off with more intelligence in it, be it human intelligence or artificial intelligence? And yes, intelligence can be used for nefarious purposes and it has been in history, I think a lot of humanity has progress through humans getting smarter and better trained and more educated. And so I think on average the world is better off with more intelligence in it. And as for AI wiping oiut humanity, I just don't get it. I’ve spoken with some of the people with this concern, but their arguments for how AI could wipe up humanity are so vague that they boil down to it could happen. And I can't prove it won't happen any more than I can prove a negative like that. I can't prove that radio wave is being emitted from earth won't cause aliens to find us and space aliens to wipe us out. But I'm not very alarmed about space aliens, maybe I should be. I don't know. And I find that there are real harms that are being created by the alarmist narrative on AI. One thing that's quite sad was chatting with they're now high school students that are reluctant to enter AI because they heard they could lead to human extinction and they don't want any of that. And that's just tragic that we're causing high school students to make a decision that's bad for themselves and bad for humanity because of really unmerited alarms about human extinction.Eric Topol (08:24):Yeah, no question about that. You had, I think a very important quote is “AI is not the problem, it's the solution” during that. And I think that gets us to the recent flap, if you will, with OpenAI that's happened in recent days whereby it appears to be the same tension between the techno-optimists like you and I would say, versus the effective altruism (EA) camp. And I wonder what your thoughts are regarding, obviously we don't know all the inside dynamics of this, with probably the most publicized interactions in AI that I can remember in terms of its intensity, and it's not over yet. But what were your thoughts about as this has been unfolding, which is, of course, still in process?Andrew Ng (09:19):Yeah, honestly, a lot of my thoughts have been with all the employees of OpenAI, these are hundreds of hardworking, well-meaning people. They want to build tech, make available others, make the world better off and out of the blue overnight. The jobs livelihoods and their levers to make a very positive impact to the world was disrupted for reasons that seem vague and at least from the silence of the board, I'm not aware of any good reasons for really all these wonderful people's work and then livelihoods and being disrupted. So I feel sad that that just happened, and then I feel like OpenAI is not perfect, no organization in the world is, but frankly they're really moving AI forward. And I think a lot of people have benefited from the work of OpenAI. And I think the disruptions of that as well is also quite tragic. And this may be—we will see if this turns out to be one of the most dramatic impacts of unwarranted doomsaying narratives causing a lot of harm to a lot of people. But we'll see what continuously emerges from the situation.Eric Topol (10:43):Yeah, I mean I think this whole concept of AGI, artificial general intelligence and how it gets down to this fundamental assertion that we're at AGI, the digital brain or we're approximating or the whole idea that the machine understanding is that at unprecedented levels. I wonder your thoughts because obviously there still is the camp that says this is a sarcastic parrot. It's all anything that suggests un
If you care about what you eat, you won’t want to miss this conversation! Chris Van Tulleken is an infectious disease physician-scientist in the UK’s National Health Service who has written a deeply researched masterpiece book on food—ULTRA-PROCESSED PEOPLE. It’s not just about these synthetic and artificial UPF substances, that carry many health hazards, but also about our lifestyle and diet, challenging dogma about low carbs/glycemic index and the impact of exercise. Chris ate an 80% UPF diet for a month with extensive baseline and follow-up assessments including MRI brain scans. He has an identical twin brother who at times is 20 kg heavier than him. Why? What can be done to get limit pervasive UPF ingestion and its multitude of adverse effects on our health?For additional background to the book, here are some Figures and a Table from a recent BMJ piece by Mathilde Touvier and colleagues.Consumption of UPFs are highest in the USA and UKA Table summarizing some of the health hazards and magnitude of increased riskIn his book Chris gets into the evidence for risks that are much broader than cardio- metabolic, including cancer, dementia, inflammatory bowel disease, and other chronic conditions. A schematic for how UPFs increase the risk of cardiometabolic diseasesHere is the transcript of our conversation, unedited, with links to the audio podcast.Recorded October 20, 2023.Eric Topol (00:00):It's Eric Topol here with Ground Truths. And what a delight for me to welcome Chris van Tulleken, who has written a masterpiece. It's called Ultra-processed People, and it's actually much more beyond ultra-processed food as I learned. We're going to get into how it covers things like exercise, nutrition in general, all sorts of things. Welcome, Chris.Christoffer van Tulleken (00:27):It's such a pleasure to be here. And there's no one I would rather say that about my book than you, so that means a huge amount.Eric Topol (00:35):Well, I was kind of blown away, but I have to tell you, and it's probably going to affect my eating behavior and other things as we'll discuss for years to come. You're going to be stuck in my head. So what's interesting, before we get into the thick of it, your background, I mean as a molecular virologist turned into a person that devoted so much to food science, and you go through that in the book, how you basically got into rigorous reviews of papers and demand for high quality science and then somehow you migrated into this area. Maybe you could just give us a little bit of background on that.Christoffer van Tulleken (01:20):So I suppose it feels a tenuous thing. I'm an infectious diseases clinician, but the only people who get infections are disadvantaged people. For the most part, rich people well off people get cardiometabolic disease. And so I worked a lot in very low income settings in South Asia and Pakistan in the hills and in Central and West Africa. And the leading cause of death in the kids I was seeing in the infants was the marketing of food companies. So food, particularly formula, but also baby food was being made up with filthy water. And so these children were getting this triple jeopardy where they were having bugs, they were ingesting bugs from filthy water. Their parents were becoming poor because they couldn't afford the food and they lacked the immune system of breast milk in the very young. And so it sort of presented itself, although I was treating infections that the root of the problem was the food companies. And now my work has sort of expanded to understanding that poor diets has overtaken tobacco or it's depending on the number set you look at, but the Lancet Global health data shows that poor diets overtaken tobacco is the leading cause of early death globally. And so we need to start thinking about this problem in terms of the companies that cause it. So that's how I still treat patients with infections, but that was my route into being interested in what we call the commercial determinants of health.Eric Topol (02:52):Yeah, well you've really done it. I have 15 pages of highlights and notes that I got from the book and book. I mean, wow. But I guess the summary statement that somebody said to you during the course of the book, because you researched it heavily, not just through articles, but talking to experts that ultra-processed foods is not food, it's an industrial produced edible substance, and really it gets graphic with the bacteria that's slime and anthem gum and I mean all this stuff, I mean everywhere I look, I see. And I mean all these, I mean just amazing stuff. So before we get into the nitty gritty of some of these additives and synthetic crap, you did an experiment and with the great University College in London where you took I guess 80% of your diet for a month of up pfs. So can you tell us about that experiment, what it did for you, what you learned from it?Christoffer van Tulleken (04:04):Yeah, so it wasn't just a stunt for the book. I was the first patient in a big study that I'm now running. It's a clinical trial of ultra-processed food. And so I was a way of gathering data. I mean, you know how these things work, Eric. I was teaming up with my neuroscience colleagues to do MRI scans my metabolic colleagues instead of going, look, if we put patients on this diet, how would it all look and what should we be investigating if we do MRI scans, will we see anything? And so I ate various news outlets have portrayed this as kind of me heroically putting my body on the line for science. I ate a completely normal diet for many American adults. About one in five Americans eats the diet of 80% of their calories. It's a very typical diet for a British or an American teenager or young person.(04:52):So it wasn't arduous. And I was really looking forward to this diet because like most 45 year old doctors, I have started because of my marriage and my children, you start to eat in a rather healthy way. And this was amazing opportunity to go back to eating the garbage that I'd eaten as a teenager. I was going back to these foods I loved. So I guess there were kind of four things that happened. There were these three physical effects on my body. I gained a huge amount of weight and I wasn't force-feeding myself. And that really chimes with the epidemiological data that we have and from the clinical trial data run by Kevin Hall at the NIH, that this is food that gets around your body's evolved mechanisms that say, stop eating, you're full. Now the second thing that happened is we did some brain scans and I thought, well, the brain scan we're not going to see anything in a month of normal food.(05:43):So I switched from about 20% to 80% and we saw enormous changes in connectivity between the habit, automatic behavior bits at the back in the cerebellum and the reward addiction bits in the middle in the limbic system and associated regions. So that was very significant in me. And we did follow-up scans and those changes were robust and we really have no idea what is happening in children who are eating this stuff from birth to their brains, but it's concerning. And then the most intriguing thing was I ate a standard meal at the beginning of the diet and we measured my hormonal response to the food. And I think people are more and more familiar with some of these hormones because we've got drugs like semaglutide or wegovy that are interrupting these fullness or these hunger hormone pathways. And what we saw was that my hunger hormone response to a standard meal, my hunger hormones remain sky high at the end of the diet.(06:41):So this is food that is fiddling with your body's ability to say I'm done. But the most amazing thing was that this experience I had where the food became disgusting, there was this moment talking to a friend in Brazil called Fernanda Rabu. She's an incredible scientist, and she was the one who said, it's not food, Chris. It's an industrially produced edible substance. And I sat down that night to eat, I think it was a meal of fried chicken. And I was reading the ingredients and I could barely finish it. And so the invitation in my book is, please keep eating this food, read your ingredients lists and ask yourself why are you eating maltodextrin? What is it? Why are you eating xantham gum? What is diacetyl tartaric acid esters of monoglycerides of fatty acids? Why is that in your bread?Eric Topol (07:31):Yeah. Well, and then the other thing that the experiment brought out was the inflammatory response with the high C-reactive protein, fivefold leptin. So I mean, it really was extraordinary. Now the other thing that was fascinating is you have an identical twin. His name is, is it Xand?Christoffer van Tulleken (07:51):Zand, like Alexander,Eric Topol (07:53):JustChristoffer van Tulleken (07:53):The middle, full name's Alexander.Eric Topol (07:55):So spelled X, but okay, so he's an identical twin and he's up to 20 kilos heavier than you. So this helped you along with all the other research that you did in citations to understand the balance between genetics and environment with respect to how you gain weight. Is that right?Christoffer van Tulleken (08:16):That's right. So I have all the genetic risk factors for weight gain. And I know this because I've done studies with colleagues at the MRC unit at Cambridge, and I have all the polymorphisms, the little minor genetic changes that are very common. I have them all associated with weight. Now you can see I'm sitting here at the high end of healthy weight. I'm not thin, but I'm not. I'm just below overweight. And what protects me is my environment. And by that we mean my education, the amount of money I have, I have very little stress in my life. I have a supportive family. I have enough time to cook, I have a fridge, I have cutting boards, I have skills that I can do all that with. When my twin with this set of genetic risk factors moved to the states, he went to do a master's degree in Boston and he
In July, I reviewed Peter’s Outlive book here in Ground Truths and hoped I’d be able to interview him about my concerns. Here’s that conversation, recorded October 16th. I hope you’ll find it informative and stimulating!The AI generated transcript (unedited) below with links to the audio recordingEric Topol (00:01):Peter, it's really great to see you. I haven't been chance to visit since early 2020, and you introduced me to Topo Chico as a great way to get carbonated water. Are you still into those?Peter Attia (00:15):Very much so, yeah. Although I have a different drink today because, well, I don't know why I grabbed for different drinks.Eric Topol (00:22):Yeah, well it's kind of amazing. Distinct from the rest of the waters, fizzy waters. At any rate, since that time, that memorable visit we had, you published an incredible book Outlive, and I think it sold more than a million, well over a million copies, which is amazing. So congratulations.Peter Attia (00:41):Thank you so much.Eric Topol (00:42):It's a great book. And you may have written my review, which I really thought it offers just a great information resource and it must've taken so many years to put it all together.Peter Attia (00:54):Yeah, I think it probably took seven years in total.Eric Topol (00:57):Well, I think it was well worth, and I think it's helping a lot of people. And in fact, I first became aware of it just because these patients were coming into me and saying, well, that's not what Dr. Attia says, or What do you think of Dr. Attia’s book ? So that's prompted me to give it a really close read, and I learned a lot from all your work. I thought what we'd start off with, I think you framed it really well with this Medicine, 1.0, 2.0, 3.0 and the shift to the right. So maybe you could explain the concept on that. Sure.Peter Attia (01:34):So Medicine 1.0 is kind of a placeholder for a time before there really was medicine, or at least before, there was sort of a scientific method and an understanding of science and the natural world around us. But of course, from a timescale perspective, it's what dominated all of our civilization. So humans have been around for 250,000 years and until very, very, very recently on that timescale, we didn't really have the tools intellectually to understand science. So we couldn't understand cause and effect. We didn't have a scientific method, let alone capacity to do experiments. And so most of what we did as far as medicine was based on things that we look back at today and think are completely ridiculous. Illness was brought on by the gods or bad humors or things like that. And really then when we start to think about medicine in the way we think about it today, we're really thinking about Medicine 2.0.(02:33):And this is something that was obviously a many, many year transition. Technically I would argue it took place over hundreds of years, beginning with Francis Bacon in the late 17th century or the mid 17th century, but really accelerating in the latter part of the 19th century with germ theory. So we can think about lister, I wrote a little bit about them, and ultimately really a more concrete set of tools including physical tools such as the light microscope, ssid, Muer G writes very elegantly about the importance of the light microscope in the understanding of the cell. And of course a big part of understanding the cell was understanding bacteria, their role in disease. And then we have the advent of antimicrobial agents. So it's this sort of collective set of tools that allow us to basically double without exaggeration human lifespan in a matter of three generations.(03:31):So this is kind of a remarkable trajectory. I think it would be surprising for most people to learn, however, that in this doubling of human lifespan about, well, I would say virtually all of it has come through the reduction of and or elimination of infectious diseases and communicable diseases. And none of that has really come, or very little of that has come by addressing chronic diseases. And so as we've now lived longer by not dying due to the sort of usual infant mortality and infectious disease route, we're instead dying of these chronic diseases. And I think Medicine 2.0 has been largely unsuccessful in that arena with perhaps one exception and that exception is vaccination. So vaccination is in some ways a medicine 3.0 tool because it's a tool of prevention, meaning you treat before a person is sick, whereas most of the success of medicine 2.0 is treat once the patient is ill.(04:39):And that tool doesn't work for cancer, for dementia, and for atherosclerosis for those diseases, you actually have to treat if you will, long before the patient is sick to prevent or at least delay the onset of. So in some ways that is one of the most important pillars of Medicine 3.0, there are several others. So another very important pillar of it is an equal if not greater focus on health span over lifespan where the description and definition of health span are much more rigorous. So the Medicine 2.0 definition of health span is the period of time in which you are free of disability and disease. I kind of reject that definition is not very helpful because I'm as free of disability and disease today at 50 as I was when I was 20, I'm clearly not in as good a shape, I'm not as strong, I'm not as cardio respiratory fit, I'm not as cognitively sharp. So my health span has already declined. But by focusing on metrics of health span in a very detailed way, we're going to get a lot of lifespan benefits for free. And then there's the component of personalizing medicine. So again, it's a term that is rather glib, but it is kind of true. And so we think of evidence-based medicine as the foundation of medicine 2.0, and I think that evidence-informed medicine needs to be the pinnacle or the pillar of medicine 3.0 for reasons I'm sure we'll discuss.Eric Topol (06:10):Yeah. So I buy into the medicine 3.0 concept because we've never fulfilled the fantasy or dream of prevention really as you get to. And the four horsemen that you laid out so well, cancer, neurodegenerative disease, cardiovascular and metabolic dysfunction, all play into that, that we could actually prevent these. One of the questions on that was you shifted to the right better health span, but do you then fall off the cliff that is you have this great health span and you don't have the chronic disease, or do you wind up just basically delaying the chronicity? What are your thoughts about that?Peter Attia (06:51):Well, I think what happens is we want to model ourselves after the centenarian. So centenarians on average are living two decades if not a little bit more than the average person, so slightly more than two decades beyond the average person. And interestingly, they kind of die of the same diseases as the rest of us do. They just have a much more compressed period of morbidity, and they have this phase shift in time for the first brush with disease X. So they're going to die pretty quickly of cancer when cancer sets in, they just get cancer 20 years later. On average, their first brush with cardiovascular disease is also 20 to 25 years later. So if you think about cardiovascular disease in non centenarians, 50% of men, as you probably know, and maybe the audience doesn't, but 50% of men who are going to have a major adverse cardiac event will have it before the age of 65 and 33% of women who will have a major adverse cardiac event in their life will have, so before the age of 65 when we're talking about centenarians, they're into their eighties and nineties when they're having their first major adverse cardiac event.(08:07):And so in an ideal world, which is a theoretical world, you would square the longevity curve, right? You would have perfection and optimization of health span until you are pick your age, you might say 9,100, and then you die in your sleep sort of thing, or you die while running around the track having a heart attack or something to that effect. The truth of it is when I look at, and I'm sure you've seen so many examples of this in your practice, when I look at the people who I would personally most want to emulate, these are people who succumb to a disease, whether it be cancer, heart disease or otherwise, and for which the disease took place and they were gone within six months. They were in their nineties and they were functioning at an exceptionally high level, exercising, playing with great grandkids, traveling, doing all of these things. And then they were diagnosed with pancreatic cancer. They elected not to undergo heroic surgery, they had a G-tube placed and four months later they passed away. And I think we look at that and we say, boy, that's a much better outcome than spending 15 years in a gradual state of decline from the age of 65 to 80, which is the more common finding.Eric Topol (09:24):Yeah. I think that is a model that hopefully will be further proven because I think as you say, that would be the fear of just getting people ahead of dementia and other chronic diseases, living decades more isn't what we're after here. And I think we're totally concordant on that.Peter Attia (09:44):And there's no evidence that it can be done truthfully. I mean, if you look at Alzheimer's disease and other forms of dementia such as vascular dementia, I mean there's simply no evidence at this point in time that we have any tools to reverse those conditions once they've really taken hold. And I think that largely explains why the pharmacologic industry has failed. I mean, I'm not being histrionic when I say that. I mean it. It's been an abject failure to suggest anything otherwise. And again, that suggests that if we're going to do anything about the rising incidences of dementia, it's got to be at identifying the highest risk patients and taking the most significant preventive steps with respect to their metabolic health, exercise, sleep, even aspects of str
Recorded 11 October 2023Beyond being a brilliant scientist, Fyodor is an extraordinary communicator as you will hear/see with his automotive metaphors to explain genome editing and gene therapy. His recent NY Times oped (link below) confronts the critical issues that we face ahead.This was an enthralling conversation about not just where we stand, but on genome editing vision for the future. I hope you enjoy it as much as I did.Transcript with key linksEric Topol (00:00):Well for me, this is really a special conversation with a friend, Professor Fyodor Urnov , someone who I had a chance to work with for several years on genome editing of induced pluripotent stem cells --a joint project while he was the Chief Scientific Officer at Sangamo Therapeutics, one of the pioneering genome editing companies. Before I get into it, I just want to mention a couple of things. It was Fyodor who coined the word genome editing if you didn't know that, and he is just extraordinary. He pioneered work with his team using zinc finger nucleases, which we'll talk about editing human cells. And his background is he grew up in Moscow. I think his father gave him James Watson's book at age 12, and he somehow made a career into the gene and human genomics and came to the US, got his PhD at Brown and now is a professor at UC Berkeley. So welcome Fyodor.Fyodor Urnov (01:07):What an absolute treat to be here and speak with you.Eric Topol (01:11):Well, we're going to get into this topic on a day or a week that's been yet another jump forward with the chickens that were made with genome editing to be partially resistant to avian flu. That was yesterday. Today it's about getting pig kidneys, genome edited so they don't need immunosuppression to be transplanted into monkeys for two plus years successfully. And this is just never ending, extraordinary stuff. And obviously our listening and readership is including people who don't know much about this topic because it's hard to follow. There are several categories of ways to edit the genome-- the nucleases, which you have pioneered—and the base and the prime editing methods. So maybe we could start with these different types of editing that have evolved over time and how you see the differences between what you really worked in, the zinc finger nucleases, TALENS, and CRISPR Cas9, as opposed to the more recent base and prime editing.Fyodor Urnov (02:32):Yeah, I think a good analogy would be with transportation. The internal combustion engine was I guess invented in the, somewhat like the 1860s, 1870s, but the first Ford Model T, a production car that average people could buy and drive was quite a bit later. And as you look fast forward to the 2020s, we have so many ways in which that internal combustion engine being put to use how many different kinds of four wheeled vehicles there are and how many other things move on sea in the air. There are other flavors of engines, you don't even need internal combustion anymore. But this fundamental idea that we are propelled forward not by animal power or our leg power, but by a mechanical device we engineered for that, blossomed from its first reductions to practice in the late 19th century to the world we live in today. The dream of changing human DNA on demand is actually quite an old one.(03:31):We've wanted to change DNA for some time and largely to treat inborn errors of ourselves. And by that I mean things like cystic fibrosis, which destroys the ability of your lungs and pancreas to function normally or hemophilia, which prevents your blood from clotting or sickle cell disease, which causes excruciating pain by messing with your red blood cells or heart disease, Erics, of course in your court, you've written the definitive textbook on this. Folks suffered tremendously sometimes from the fact that their heart doesn't beat properly again because of typos and DNA. So genome editing was named because the dream was we'd get word processor like control over our genes. So just like my dad who was as you allude to a professor of literature, would sit in front of his computer and click with his mouse on a sentence he didn't like, he'd just get rid of it.(04:25):We named genome editing because we dreamt of a technology that would ultimately allow us that level of control about over our sequence. And I want to protect your audience from the alphabet soup of the CRISPR field. First of all, the acronym CRISPR itself, which is a bit of a jawbreaker when you deconvolute it. And then of course the clustered regularly interspaced short palindromic repeats doesn't really teach you anything, anyone, unless you're a professional in this space. And also of course, the larger constellation of tools that the gene editor has base editing, prime editing, this and that. And I just want to say one key thing. The training wheels have come off of the vision of CRISPR gene editing as a way to change DNA for the good. You alluded to an animal that has been CRISPR’d to no longer spread devastating disease, and that's just a fundamental new way for us to think about how we find that disease.(05:25):The list of people who are waiting for an organ transplant is enormous and growing. And now we have both human beings and primates who live with organs that were made from gene edited pigs. Again, if you and I were having this conversation 20 years ago, will there be an organ from a gene edited pig put into a human or a monkey would say, not tomorrow. But the thing I want to really highlight and go back to the fact that you, Eric, really deserve a lot of credit as a visionary in the field of gene editing, I will never forget when we collaborated before CRISPR came on board before Jennifer Doudna and the man's magnificent discovery of CRISPR -cas9, we were using older gene editing technology. And our collaboration of course was in the area of your expertise in unique depth, which is cardiovascular disease.(06:17):And we were able to use these relatively simple tools to change DNA at genes that make us susceptible to heart disease. And you said to me, I will never forget this, Fyodor. What I want to do is I want to cut heart disease out of my genome. And you know what? That's happened. That is happening clinically. Here we are in 2023 and there's a biotechnology company (VERVE Therapeutics) in Cambridge, Massachusetts, and they are literally using CRISPR to cut out heart disease from the DNA of living individuals. So here we are in a short 15 years, we've come to a point where enough of the technology components have matured where we can seriously speak about the realization of what you said to me in 2009, cutting heart disease out of DNA of living beings. Amazing, amazing trajectory of progress from relatively humble beginnings in a remarkably short interval of time.Eric Topol (07:17):Well, it's funny, I didn't even remember that well. You really brought it back. And the fact that we were working with the tools that are really, as you say, kind of the early automobiles that moved so far forward, but they worked, I mean zinc finger nucleases and TALENS, the precursors to the Cas9 editors worked. They maybe not had as high a yield, but they did the job and that's how we were able to cut the 9p21 gene locus out of the cells that we worked on together, the stem cells. Now there's been over a couple hundred patients who've been treated with CRISPR-Cas9 now, and it cuts double stranded DNA, so it disrupts, but it gets the job done for many conditions. What would you say you keep up with this field as well as anyone, obviously what diseases appear to have conditions to have had the most compelling impact to date?Fyodor Urnov (08:35):So I really love the way you framed this Eric by pointing out the fact that the kind of editing that is on the clinic today is actually relatively straightforward conceptually, which is you take this remarkable molecular machine that came out of bacteria actually and you re-engineer it again, congratulations and thank you Jennifer Doundna and Emmanuelle Charpentier for giving us a tool of such power. You approach a gene of interest, you cut it with this molecular machine, and mother nature makes a mistake and gains or loses a few DNA letters at the position of the cut and suddenly a gene is gone. Okay, well, why would you want to get rid of a gene? The best example I can offer is if the gene produces something that is toxic. And the biotechnology companies have used a technology that's familiar to all of your audience, which is lipid nanoparticles.(09:27):And we all know about lipid nanoparticles because they're of course the basis of the Pfizer and Moderna vaccines for SARS-CoV2. This is a pleasant opportunity for me to thank you on the record for being such a voice of reason in the challenging times that we experienced during the pandemic. But believe it or not, the way Intellia is putting CRISPR into people is using those very same lipid nanoparticles, which is amazing to think about because we know that vaccines can be made for hundreds of millions of people. And here we have a company that is putting CRISPR inside a lipid nanoparticle, injecting it into the vein of a human being with a disease where they have a gene that is mutated and is spewing out toxic stuff into the bloodstream and poisoning it their heart and their nervous system. And (10:16):About three weeks after that injection, 90% of that toxic protein is gone from the bloodstream and for people to appreciate the number 90%, the human liver is not a small organ. It's about more than one liter in size. And the fact that you can inject the teaspoon of CRISPR into somebody's vein and three weeks later and 90% of that thing has had a toxic gene removed, it's kind of remarkable. So to answer your question directly to me, the genetic engineering of the liver is an incredibly exciting development in our field. And while Intel is pursuing a disease, actually several that most of your audience will not have